The Trump regime used veterans as guinea pigs.
SPRING CITY, Pa. — They wrapped the dead in body bags and raced back to treat the living, crammed into a nursing home that, day after day, played the somber sound of taps over the speaker system so the veterans who lived there had the chance to say goodbye.
The nurses and aides at the Southeastern Veterans’ Center in the suburbs of Philadelphia had watched so much go wrong since the start of the coronavirus pandemic. The communal dining that lasted into April, the nights that feverish patients were left to sleep beside roommates who weren’t sick yet. “Merry Christmas,” one nurse told another when they finally got N95 masks, weeks into the crisis and just before administrators stopped staffing the isolation rooms because too many people were feared infected.
But what worried some nurses most was what they called the “covid cocktail,” the widespread, off-label use of one of the antimalarial drugs touted by President Trump in March as a potentially game-changing treatment for covid-19.
For more than two weeks in April, a drug regimen that included hydroxychloroquine was routinely dispensed at the struggling center, often for patients who had not been tested for covid-19 and for those who suffered from medical conditions known to raise the risk of dangerous side effects, interviews, emails and medical notes and records obtained by The Washington Post show.
Though precise estimates vary, the state Department of Military and Veterans Affairs said about 30 residents received the drug. Several nursing home staff members placed the number higher. The Chester County coroner, who reviewed the medical records for some of those who died, said at least 11 residents who had received the hydroxychloroquine treatment had not been tested for covid-19.
The drug regimen appeared to conflict with guidance from the Food and Drug Administration, which issued an emergency-use authorization for the drugs in late March but stressed they should be administered only during clinical trials or in hospitals providing “careful heart monitoring” and only after detailed discussions with patients and families about the risks. At the 238-bed nursing home, the treatment was given over the objections of some nurses, at times with little knowledge among patients’ families and largely hidden from lawmakers who have been probing the matter, according to interviews and emails.
“Started on the Covid Cocktail,” the center’s records noted for an 86-year-old resident with a history of arrhythmia, resulting in a pacemaker placement.
“Prophylactic,” the records said in describing the preventive regimen of hydroxychloroquine for a woman in her 80s who had a cough and was running a fever of 100.4.
The home’s interim commandant, Barbara Raymond, who took over after the treatment ended, declined to comment. Michele Shrikanthan, the center’s medical director, and Rohan Blackwood, the home’s commandant at the time, did not return calls.
State officials said health-care providers at the center had sole discretion on use of the drug. The medical director and another doctor, along with two nurse practitioners, write prescriptions at the home.
“Leadership was aware of [hydroxycholoroquine] being prescribed for residents,” said Joseph Butera, deputy communications director for the Pennsylvania Department of Military and Veterans Affairs, which operates Southeastern and five other state homes for veterans. “It was up to providers as to whether they felt comfortable.”
In May, the state suspended Blackwood and the center’s director of nursing after the Philadelphia Inquirer reported widespread breakdowns at the facility and the use of hydroxychloroquine at that home and others. Dozens of emails, reports, medical notes and records as well as interviews with 17 nurses, family members, doctors and others by The Post show how broadly the home turned to the unproven treatment and how a complex state bureaucracy went on to obscure critical decision-making in the midst of a pandemic.
The center and the two state agencies responsible for oversight have released little information about what transpired. The Department of Military and Veterans Affairs has confirmed the use of the drug but has not offered details about what led the doctors on-site to decide to use it. The state Department of Health, which inspected the home on May 1 and did not cite a single deficiency in infection control or patient care, declined to say whether hydroxychloroquine was administered. The center has released no information about how patients were selected or monitored.
“I am absolutely gobsmacked about the events that have occurred there,” said William C. Hunter, a Johns Hopkins-trained internist who served as the center’s medical director until he retired in December. “It was an untried cocktail. The risks and potential benefits were completely unknown — no real scientific studies were conducted.”
Hunter, who said he has been talking to staff at the home for weeks, called the treatment “reckless.”
“My sense,” he said, “is that things were starting to spiral out of control and they were looking for a magic bullet. It was horrifying.”
Nurses who had spent years caring for veterans and their spouses at Southeastern said they raised concerns. Without covid-19 testing, they said, potentially virus-free patients in their 80s and 90s were at risk of being dosed with an unproven drug they didn’t need or, worse yet, could hurt them.
“Why are we giving this to them?” one nurse recalled asking Shrikanthan after several residents with heart problems were placed on the drug regimen. Like five other caregivers at the home, the nurse spoke to The Post on the condition of anonymity to freely discuss what happened.
In response to the inquiry, the nurse said she was told, “This is the standard order.”
“I felt like I was playing Ring Around the Rosie,” she said. “Nobody wanted to sit and explain why. If that were my mom or dad, I would want answers.”
Another staff member decided to keep a running list of residents who were administered the drugs and counted nearly three dozen. The Post did not have access to the records needed to independently corroborate the numbers.
The cocktail included azithromycin, commonly used to treat infections, and Plaquenil, a brand name for hydroxychloroquine, a sampling of medical records obtained by The Post show.
Doctors “would just give it without any parameters,” the staff member who kept the tally said. “We weren’t monitoring … as much as we needed to.”
There is no way to know whether the treatment played a role in any of the deaths at the home, which has attributed 42 fatalities to covid-19. Chester County Coroner Christina VandePol, a board-certified internist trained at the University of Pennsylvania, said the center signed off on the death certificates of residents and, in many cases, sent the bodies to funeral homes outside the area.
Through medical records and reports from the home, VandePol said, she determined that at least 14 residents whose deaths were tied to covid-19 were never actually tested for the infection. Of those, 11 had been given hydroxychloroquine before they died, she said. VandePol is pressing to have all nursing home deaths reported to the state’s coroners moving forward.
“In the case of hydroxychloroquine, as part of a covid cocktail, perhaps, knowing there would be outside scrutiny, the home would not have been as cavalier about routinely giving elderly debilitated people an unproven drug outside of a clinical trial,” she said.
The center stopped administering the drug around April 22, according to an email obtained by The Post that was sent to more than a dozen staff members. Earlier that week, a nationwide study of 368 hospitalized Veterans Affairs patients with covid-19 reported that the death rate was higher for those treated with hydroxychloroquine.
“The providers have decided not to use this drug anymore,” Deborah Mullane, then the center’s director of nursing, wrote in the email. “All current Plaquenil orders have been discontinued.”
Last month, the FDA reported that the antimalarial drugs had triggered cardiac problems and other adverse effects in covid-19 patients and revoked the emergency-use authorization, which had allowed the transfer of funds to the Strategic National Stockpile for distribution of the drugs to hospitals.
Families and staff members are still grasping for an explanation. In recent weeks, more than 40 people have reached out to state Sen. Katie Muth (D), who lives two miles from the home and has been heading up an unofficial investigation. Answers have been hard to come by.
In response to an inquiry from Muth last month, state Health Department legislative director David Toth defended the use of hydroxychloroquine but declined to say whether it was actually ever used.
“In late March, numerous sources began highlighting a potential benefit of the use of hydroxychloroquine and chloroquine for covid-19,” he said in an email written on behalf of Health Secretary Rachel Levine, whose agency is responsible for ensuring the home meets federal health and safety standards. “Health care providers throughout the country began to use this medication to treat covid-19 patients based on that literature. At that time, the federal government also touted its potential benefit. This was an off-label use of the medication, but it is important to note that doctors can and do write off-label prescriptions for FDA-approved medications.”
Without clarity from state agencies, Muth has called on the state attorney general to investigate.
“I sort of Forrest Gump-ed myself into finding out about the use of Plaquenil,” the 36-year-old lawmaker said. “I knew a lot of really horrible stuff was happening there, all these deaths, but I didn’t know this. … Did they die from the drug? Did they die from covid? What did they die from?”
Chaos, questions, deaths
Residents and their family members had no idea how many people were dying at the four-story veterans’ home near the Schuylkill River when the Philadelphia Inquirer broke a story on April 25. The news was stunning: 26 residents had died in what had clearly become one of the deadliest coronavirus outbreaks in the state.
Inside the home, staff members said, they were pleading to wear personal protective equipment, isolate the sick and keep nurses and aides who had been exposed to the virus away from healthy patients. The sounds of coughing swept the hallways and the activity rooms, where residents shared colored pencils and dice. Those who grew too ill to eat sat listless over ham loaf alongside healthier residents in the dining hall.
“We were handing out Tylenol like crazy,” one nurse said. “There were times when I would stand there peeing on myself because I had so many sick people and you just couldn’t take the time to stop.”
As staff members scrambled to control the rapid-fire spread of infection, the center turned to hydroxychloroquine.
Trump started talking about antimalarial drugs in mid-March, suggesting a potential, off-label treatment for covid-19, which has so far killed at least 42,000 nursing home residents nationwide. Public health experts urged extreme caution, saying the drugs were unproven and could potentially trigger life-threatening side effects, particularly in cardiac patients.
“We do not know if it works for covid-19,” the FDA wrote in March when it authorized the use of the drugs. “There is limited information known about the safety and effectiveness (whether this will make you better).”
The president pressed forward during a series of televised press briefings. “It’s a very strong, powerful medicine, but it doesn’t kill people,” Trump declared in early April. “We have some very good results and some very good tests.”
The FDA made clear the treatment should be used in hospitals, which can provide intense monitoring. Some have deployed teams that include cardiologists, electrophysiologists, infectious-disease physicians, pharmacists and nurses.
“It was a multidisciplinary effort to make sure that if this was used, everyone was making sure it was being used as safely as possible,” said Barbara Santevecchi, an infectious-diseases clinical pharmacy specialist and professor in the Department of Pharmacotherapy and Translational Research at the University of Florida. “You have to be able to watch for adverse effects.”
The Centers for Medicare and Medicaid Services, which regulates the 15,000 nursing homes in the United States, has provided no guidance on the use of the drugs in nursing homes since Trump first touted the potential benefits. Local media have reported that nursing homes in Texas, Illinois, Connecticut and North Carolina treated patients with the drugs.
The Southeastern center ordered hydroxychloroquine from a wholesale pharmacy in March and notified the state Department of Military and Veterans Affairs when health-care workers started administering the drug in April, said Butera, the department’s deputy communications director. Darryl Jackson, the department’s chief medical officer, “ensured the medication was available in case the primary care providers at the homes felt that it was medically necessary,” Butera said in an email.
“There were numerous [Department of Health]/medical reports about the use of this drug across Pennsylvania and throughout the United States,” Butera said.
Muth, the state senator, said it appeared the home focused more on the drug supply than face masks and other protective equipment for front-line caregivers.
“Funny how they didn’t have PPE stockpiled but they made it a priority of their treatment protocol to include a drug that wasn’t proven to work and shouldn’t be used in non-hospital settings,” she said.
Nurses at Southeastern said they received little information about the new course of treatment.
“All they said was that they were starting these residents on Plaquenil. I started asking them, ‘Well, what’s Plaquenil for?’ ” one nurse recalled. “I started looking it up. We were always taught in nursing school that you’re supposed to know what medications you are giving, what it’s for and what the side effects are. I said, ‘Well, I don’t understand. Why are we giving it to the elderly?’ ”
“This is what’s ordered. This is what you’re supposed to give,” the nurse recalled being told by Shrikanthan, the center’s medical director.
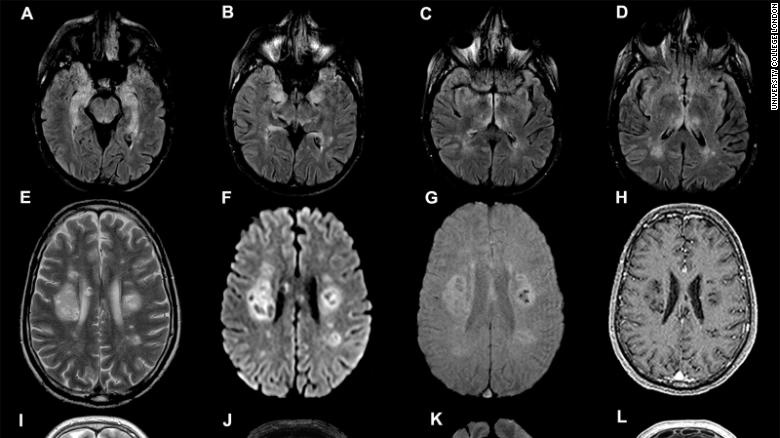
In the past, nurses said, doctors at the center had provided explicit instructions for medications that could have adverse effects. In the case of hydroxychloroquine, nurses said they were given standard orders: five days of treatment, even for patients with heart problems. Hydroxychloroquine has been found to cause serious heart irregularities, such as life-threatening arrhythmias, in covid-19 patients.
“We all started looking it up and we found that this wreaks havoc on your system,” another nurse said. “You’re talking about people with pacemakers, people with [arrhythmia] … and we’re giving it to them without any parameters. It was just like we were starting them on any other medication.”
The nurses said they raised questions but did not push the doctors or top administrators further. In interviews with The Post and in emails to Muth, staff members said they feared for their jobs, especially since the center appeared to have unwavering support from the state Department of Military and Veterans Affairs and the state Department of Health.
Health Department inspectors gave the home an overall five-star rating, the highest mark, according to a federal government rating system that takes into account quality and staffing, among other measures, records show. An inspection on May 1, days after the hydroxychloroquine treatment ended, found no violations, records show.
“That so-called DOH [inspector] was just sitting in a room talking for a few hours and they didn’t walk onto any floors nor did they speak to any staff,” one staff member wrote in an email to Muth a week after the inspection.
Nate Wardle, spokesperson for the state Department of Health, said in an email that the department “takes seriously our job of protecting the health and well-being of our most vulnerable Pennsylvanians.”
It is unclear how patients were chosen for the drug regimen. Nurses said they were instructed to give the drugs to anyone with covid-19 symptoms, including those who had not been tested for the infection.
In emails to families and in discussions with nurses, the center attributed the lack of testing to guidance from county health authorities.
According to the center, the Chester County Health Department had ordered no further testing once two or more residents in the same unit tested positive. Instead, everyone else would be considered exposed and, if symptoms developed, presumed positive without laboratory confirmation.
“Chester County stated if we have a unit who has 2 or more people who have tested + that we should presume everyone to be positive and no one additional on that floor will be tested (we tested the 3 residents before we received this directive),” a social worker at the center wrote in an April 8 email to the daughter of a resident. “At this point, everyone including Dad is presumed positive.”
A Chester County Health Department spokesperson acknowledged that in the early stages of the pandemic when supplies were limited, congregate care facilities “where some individuals tested positive could operate as if everyone who was symptomatic was also positive and should be treated as such.” The county was taking direction from the state, spokesperson Becky Brain said.
“The Chester County Health Department was following guidance from the PA Department of Health — not just for [Southeastern], but for all congregate care settings,” she said.
Wardle said the state Health Department did not order nursing homes to consider patients presumed positive for covid-19 without testing. “The department encouraged testing of symptomatic residents once an outbreak was identified,” he said.
One nurse at Southeastern said she grew particularly concerned about a resident with a low-grade fever who was presumed positive, moved into a room with two sick roommates and given Plaquenil. Before the pandemic, the man had often developed fevers from heart problems and blood clots in his legs. Suddenly, she said, he was placed alongside sick people and given a drug with potentially dangerous side effects.
“What if it’s something totally different and you just put him in isolation with two positive people … not even testing him?” she said. “Then they start him on Plaquenil.”
He later died, the nurse said.
A nursing assistant recalled the case of an elderly woman with bronchitis who was placed on the drug. Records from the home said the cocktail was given for prophylactic use.
She later died, the nursing assistant said.
“I just feel as though arrogance and ignorance came into play,” she said. “Granted, nobody really knows anything about covid, but I feel like they were more trying to cover themselves than really helping our residents at the end of the day, and it’s heartbreaking.”
‘It’s just not acceptable’
The relatives of several residents dosed with the drug say they were provided little information about the experimental course of treatment.
Long-standing federal rules on the rights of residents in nursing homes require doctors to inform patients in advance about medication changes and discuss the risks, benefits and treatment alternatives. If patients have dementia or other cognitive impairments, homes are supposed to reach out to a primary point of contact, such as a spouse or child.
Family members say the calls they received from the home about the drug treatment were brief and lacked critical details.
Before he fell ill in mid-April, 87-year-old Paul Ferko had known for days that something was very wrong at his home of nine months.
“He heard the taps,” said his daughter, Chrissy Diaz. “He told us that the virus that was on TV was in the home.”
Diaz said she received a call from the center on April 19, noting that her father was being placed on Plaquenil. She said she grew concerned because her father, a steelworker who had serviced airplanes during the Korean War, had hypertension and other medical conditions.
“They weren’t asking me in any way, shape or form,” Diaz said. “I asked if Plaquenil was hydroxychloroquine. They said it was and I asked about the side effects. I thought it was just used in hospitals. They said nursing homes could use it. They assured me that it was safe, that the side effects were minimal.”
Diaz said her father had not been tested for covid-19 when the treatment began. Medical records show he was running a fever of 99.2 and had a possible case of pneumonia. She saw him for the last time a few days later, propped up against a second-floor window by several aides. He died in a nearby hospital.
“They started using [hydroxychloroquine] on anyone who had symptoms,” Diaz said. “It was in the news. It was like the next great thing. I feel like it was, ‘Let’s use this on our elderly patients and see what happens.’ Maybe they thought they were going to die anyway. I don’t know what was going through their heads. That’s what’s really scary.”
Carol Lewis said her family received a similar call from the center and also grew concerned about the course of treatment. Her father, a computer engineer who served in the Army, had a history of heart problems, she said.
Lewis said the family instructed the center not to use hydroxychloroquine. After her father died on April 13, Lewis requested the medical records and found a doctor’s note indicating that a course of Plaquenil had been completed.
“It’s just disgraceful,” she said. “I want to know who ordered this, first of all. What happened and where was the breakdown that this whole situation went up in flames like this?”
Nursing home experts say patients and their families should have been consulted before the drugs were used and given detailed information about the potential risks and side effects.
“It’s just not acceptable. Facilities aren’t supposed to just give people drugs,” said Toby Edelman, senior policy attorney for the Center for Medicare Advocacy, a nonprofit watchdog and advocacy organization headquartered in Connecticut and Washington, D.C. “Just because it’s an emergency, facilities can’t give residents drugs that are totally unknown, untested and unproven.”
‘A closed-loop system’
Lawmakers, staff members and relatives of the deceased say state regulators have frustrated efforts to probe what happened at the home. Dozens have reached out to Muth, who had been planning to run a bingo game at the center before it was locked down to visitors in March.
“I first heard about him receiving these drugs after they were prescribed and administered with no idea of the risks associated with other preexisting conditions,” the widow of a retired Army officer emailed on May 5. “Why did this happen out of protocol and in this case only? Was this some type of clinical trial or practice test administered to someone that could not engage in his own decision-making or were they just desperate or both?”
Muth called VandePol, the county coroner, who had not heard about the treatment. VandePol started researching the possibility that the residents had been part of an approved clinical trial. No trial existed. VandePol delved deeper, counting 14 residents whose deaths were categorized by the center as “presumed covid-19″ because they had not been tested for the infection.
“I was very surprised to find [hydroxycholoroquine] was being used in an unmonitored way for very elderly people who in some cases had not been tested for covid-19,” said VandePol, who spent more than 20 years conducting pharmaceutical trials.
Other nursing homes in the county allowed VandePol to do postmortem covid-19 tests. Bodies at the veterans’ center, however, were in most cases already released to funeral homes outside the county.
“Their institution became a closed-loop system,” VandePol said. “The people that are taking care of the patients are also certifying what the cause of death is.”
Muth blames a state system that is “internally regulated with no guarantee of transparency,” from the doctors and the director at the Department of Military and Veterans Affairs to the inspectors and the secretary at the Department of the Health.
In late May, the governor’s Office of General Counsel engaged outside counsel to conduct an independent investigation of the outbreak at the center and the way the home and the state Department of Military and Veterans Affairs addressed the crisis. No details have been released.
Amid the ongoing questions and calls for additional investigations, staff members say they are still reeling from all they saw and heard: The dead rolled into body bags with their names on toe tags and the ever-present, unwelcome sound of taps on the speaker system, notice of yet another death. Standing alongside their nurses and listening to the bugles play, residents with dementia who often could not remember what they had for dinner the night before would slowly remove their hats.
And then they would salute.