I recall a lot of contesting info early on that got drowned out. These articles also seem to follow aspects of this:
Thanks @macro for your detailed descriptions on how scrupulous NZ has been with those entering the country, the ‘managed’ isolations prior to being let in, as well as the phases of testing for Covid. What strikes me is of course that stringent adherence to those quarantine-type guidelines has kept NZ virtually safe, with very minor deaths attributed. The restrictions have benefited the country, and you guys stand out as models for what to do.
As for the 3 Covid cases due to frozen foods as a direct link to getting the virus into the country, it is a result of maximizing your careful scientific approach to ferreting out all known sources of the virus. Scientific logic prevails. Wow.
And for all the US efforts or lack thereof, it is so befuddling to fall so short to contain this pandemic through interventions and results in one of our worst epic fails. But we have to stand up daily to the lack of leadership, and try to stay safe within our very lackluster approach.
Thankfully where I live, California we do throw out mandates of steering clear of crowds, wearing masks, social distancing, and living in tiers of what’s safe and what’s not right now. But the wild card approach from those who think nothing of a 'lil flu-like virus, and want to party with major wins with basketball and baseball, thinking it’s ok to gather with friends is infuriating.
The words ‘it’s going to get worse in the fall’ are words that are coming true unfortunately.
Thanks for filling us in on how it’s supposed to work. 

Spreader event…North Carolina.
Astronomical numbers…and today another one. 
The Pandemic Is in Uncharted Territory
The fall surge is rewriting the coronavirus record books across America. And the numbers are still climbing.
The United States set a new record for reported cases this week, breaking 500,000 for the first time in the pandemic as the third surge continued to build across nearly every state in the country.
Today, the country recorded 88,452 new cases of COVID-19, its highest single-day total since the pandemic began. Over the past two weeks, 25 states have set a new record for cases in the past two weeks, including 17 states with record highs since last Wednesday.
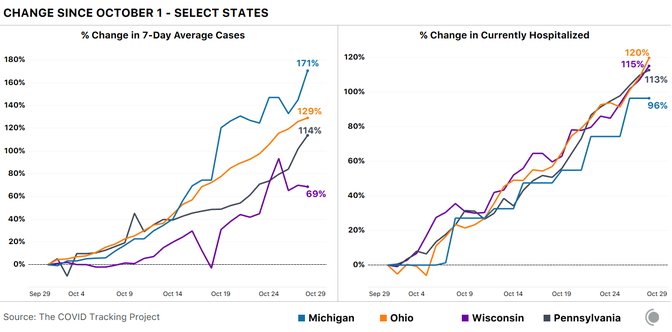
The country reported a record number of tests, at 8.2 million, but case growth (24 percent) far outpaced test growth (9 percent), as we explained earlier this week. That’s also true for the entire month of October: Forty-seven of the 50 states, along with the District of Columbia, have seen cases rise faster than reported tests since October 1.
These cases are translating into higher numbers of COVID-19 hospitalizations in many states in every region of the country. All but 11 states saw a rise in people hospitalized this week, the largest increases occurring in the upper Midwest and Texas. Although we are not yet close to the hospitalization peaks of almost 60,000 that we observed in the spring and summer, the average number of people hospitalized this week rose to 42,621, a very substantial increase from the lows of about 30,000 that we saw just a month ago.
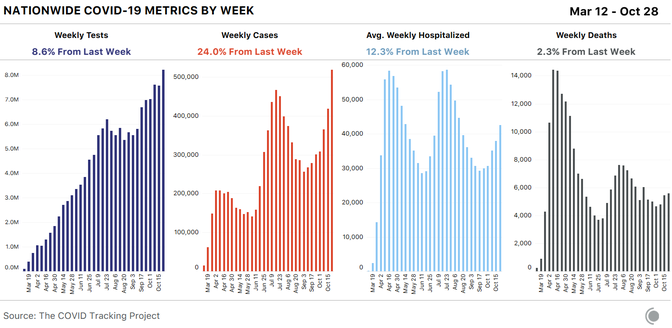
In some worrying states—North Dakota, South Dakota, and Wisconsin—hospitalization rates are approaching those of the Sun Belt–surge hot spots over the summer. At this point, we see no evidence that any state in the current surge has reached its peak and begun to decline.
COVID-19 deaths have risen, but not nearly as sharply as hospitalizations. The current explosion of cases is only three weeks old, and we know from the data that reported deaths lag behind cases and hospitalizations. According to the Centers for Disease Control and Prevention, the approximate timeline from symptom onset to the reporting of a death to public-health authorities is about three weeks, on average. This lag varies by state, and some states such as Florida take an average of more than six weeks to log COVID-19 deaths. Given the current trends, we should expect deaths to continue to rise in the coming weeks.
More encouraging, as our team explained this week, the fatality rate for hospitalized patients has declined as treatments have improved and younger and healthier people have made up more of those hospitalizations.
It’s important to note, though, that the hardest-hit states are seeing notable increases in deaths. In Wisconsin, the state that led off this surge, deaths rose 56 percent this week and are up 270 percent since the week ending October 1. Deaths have also climbed markedly in the Dakotas to a combined 101 this week, from 11 in the week ending September 3. On a per-capita basis, that is worse than any individual week of deaths in Florida at any time in the pandemic.
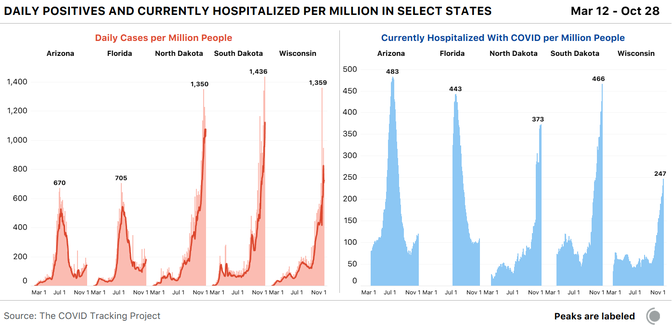
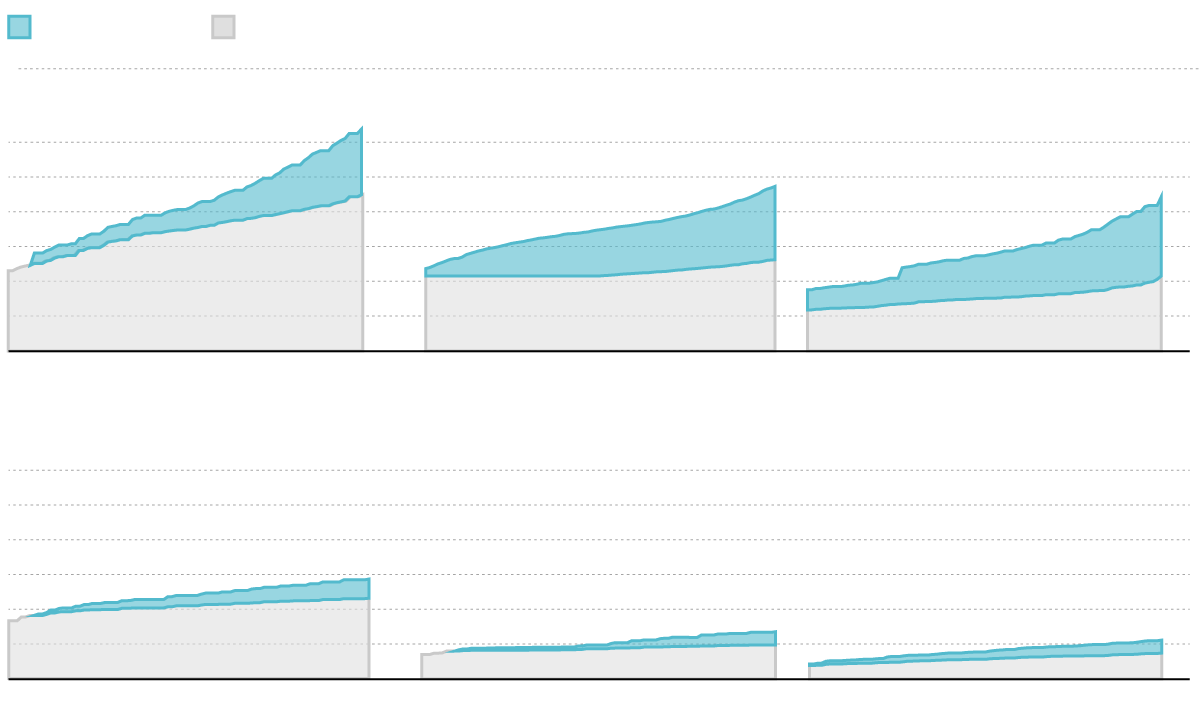
With the presidential election next week, the swing states of Michigan, Ohio, Pennsylvania, and Wisconsin would already have been in the spotlight. But they also happen to be in the midst of a major uptick in COVID-19 cases. Beyond the large rises in cases since October 1, hospitalizations are up at least 96 percent in all four states. Ohio and Wisconsin have also surpassed their previous hospitalization records.
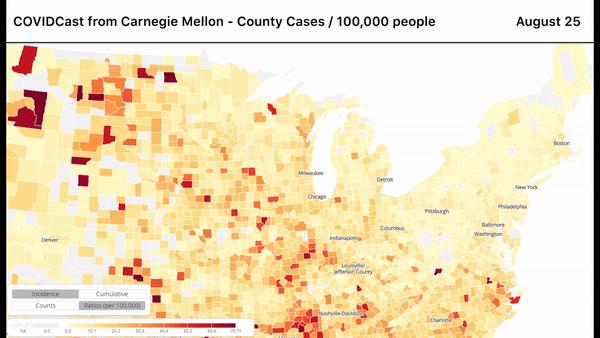
If we look at the county-level data from these four states, we see another pattern emerge. In the early days of the pandemic, the outbreaks in these states were concentrated in major cities, especially Detroit and Philadelphia, but this new surge is much more geographically dispersed.
Since September, the racial composition of people who are confirmed to have the coronavirus has also changed remarkably in the three worst-hit states, North Dakota, South Dakota, and Wisconsin. Our COVID Racial Data Tracker shows that the per-capita infection rate in Black, Latinx, and Asian communities has declined, while per-capita infections among white people have risen very slightly. (In states with mostly white populations, even a small rise in per-capita cases among white residents can translate to large increases in total numbers of cases in this population.)
In absolute terms, the disparities remain pronounced: In North Dakota, since the start of the pandemic, one in every 12 Black people has tested positive for COVID-19, compared with one in 29 white people. In South Dakota, one in every 14 Indigenous people has tested positive, compared with one in 26 white people. In Wisconsin, one in every 13 Latinx people has tested positive for COVID-19, compared with one in 30 white people. But recent data suggest that the virus is now circulating in whiter populations outside the major cities.
We’re seeing a dramatic rise in long-term-care-facility cases in many of the states now experiencing surges, an alarming trend given that long-term-care deaths account for roughly 41 percent of all COVID-19 deaths in the U.S. This week saw 17,848 new cases associated with long-term care facilities. Because many states do not separate out resident cases and staff cases, this total includes both.
Wyoming reported a record number of new cases in long-term care facilities for the third week in a row. The state has reported 309 total resident and staff cases since the beginning of the pandemic. About one-quarter of those are from this past week, and half are from the past two weeks.
Ohio reported 791 new cases of COVID-19 among nursing-home residents this week, the highest number in the state since we started tracking cases in late May. And Wisconsin’s long-term care facilities reported their highest number of resident and staff cases since May: 241.
We continue to be alarmed that Arizona and South Dakota do not report comprehensive long-term-care data. Arizona releases the number of affected facilities but does not provide facility-level case or death numbers. And South Dakota does not release COVID-19 data on long-term care facilities at all.
The bottom line this week is simple: The third surge is in full swing, hospitalizations are rising nationwide, and deaths have begun to increase in Wisconsin, the state that could be seen as the canary in the coal mine of this surge. But it is difficult to predict what might happen from here. Just as the summer surge in the Sun Belt unfolded differently than the spring outbreak in the Northeast, we are seeing distinct patterns emerge at this stage of the pandemic. Cases and hospitalizations are more geographically dispersed and appear to be rising less steeply but over longer periods. And the behavioral shifts brought on by the intense cold arriving in the upper Midwest may accelerate the spread of the virus.
Testing accessibility and in-hospital patient care have improved, so it seems unlikely that we’ll return to the case-fatality rates of the spring. The lower death rates from COVID-19, however, are predicated on stable and functioning health-care systems. As this outbreak continues to grow in so many urban and rural communities, public-health officials have brought back the “Flatten the curve” mantra of the spring. Each fall, hospitals prepare for an increase in patients requiring respiratory support due to influenza season.
What was true in the spring is true now: If hospitals are overwhelmed with COVID-19 patients, they cannot provide the quality of care that has reduced the number of Americans who die from this disease, and from other health emergencies. And local reporting suggests that communities from El Paso to Green Bay are in danger of letting the virus grow beyond the capacity of health-care workers to contain the damage.
Covid nurse death toll now as high as the number of nurses who died during World War One
Lack of proper data on deaths among healthcare workers a ‘scandal’, says international nursing chief
As many nurses have now died from coronavirus than were killed during the entirety of the First World War, the International Council of Nurses (ICN) has revealed.
The latest figures collated by the federation of 130 national nurses’ associations show that 1,500 nurses have lost their lives since the pandemic began around the world.
This is the same as the number of nurses believed to have been killed during the four years of World War One.
However, the ICN expects the figure of 1,500 to be a significant underestimate, as it only includes those who have died in 44 countries where data was available.
“The fact that as many nurses have died during this pandemic as died during World War I is shocking”, the federation’s chief executive Howard Catton said during an online conference earlier this week.
“Since May 2020 we have been calling for the standardised and systematic collection of data on healthcare worker infections and deaths, and the fact that is still not happening is a scandal.”
Separate analysis of global infection rates by the ICN suggests at least 20,000 healthcare workers have died in total from Covid, although this is only an extrapolation as concrete numbers do not exist.
Mr Catton said Florence Nightingale, the founder of modern nursing who was born 200 years ago this year, would have been angry at how little effort was being made to properly catalogue the toll the pandemic is taking on healthcare workers.
“2020 is the International Year of the Nurse and Midwife, and the 200th anniversary of Florence Nightingale’s birth, and I am sure she would have been immensely saddened and angry about this lack of data - I know I am.
“Florence demonstrated during the Crimean War how the collection and analysis of data can improve our understanding of risks to health, improve clinical practices and save lives, and that includes nurses and healthcare workers.
“If she were alive today, world leaders would have her voice ringing in their ears saying they must protect our nurses. There is a chasm between the warm words and accolades, and the action that needs to be taken.”
When the coronavirus crisis does finally come to an end, nurses must be at the forefront of rebuilding a better global health system, he added.
“When this is over, we must never take our health systems for granted again, and we must invest much more heavily in them and our health workers.
“Nurses are angry about the lack of preparedness, but they are also angry about the lack of support that they have received.”
In the UK, some nurses are warning the NHS must adapt its approach for the coming second wave of coronavirus.
Jess Moorhouse, an intensive care nurse who worked in the London Nightingale emergency hospital through its operational life, said ratios of nurses to critically ill patients had to be improved.
In normal times, there is one nurse for every patient in intensive care, but in the Nightingale this fell to one nurse for every six patients, she explained in an article for the Royal College of Nursing’s (RCN) magazine.
If this cannot be improved upon during a second surge, nurses will need to be trained to manage teams of clinicians and to delegate tasks, rather than solely focusing on practical nursing of patients, she argued.
Furthermore, the burden on nurses will be even greater as the NHS does not intend to cancel all non-Covid treatment as it did during the first lockdown.
The RCN is calling for not only more nurses trained for critical care, but also a 12.5% pay rise for the profession, arguing the pandemic has shown how essential nursing is.
“The Covid-19 crisis has given the government an historic opportunity to right some wrongs on how nursing is valued,” said the college’s chief executive Donna Kinnair. “For many years, our pay hasn’t reflected our worth. It is time for nursing staff to be paid fairly.”
What people are not paying attention to is how devastating even a moderate case can be. My daughter in law is a long hauler since mid March. She still has varying degrees of energy & radiating pain issues. It has attacked the veins in her legs & she will have surgery soon to strip them.
And we won’t know what long term issues will arise for years! Talk about pre existing conditions.
Fauci is being blunt about what he says is going wrong with our national Covid problem.
President Trump’s repeated assertions the United States is “rounding the turn” on the novel coronavirus have increasingly alarmed the government’s top health experts, who say the country is heading into a long and potentially deadly winter with an unprepared government unwilling to make tough choices.
“We’re in for a whole lot of hurt. It’s not a good situation,” Anthony S. Fauci, the country’s leading infectious-disease expert, said in a wide-ranging interview late Friday. “All the stars are aligned in the wrong place as you go into the fall and winter season, with people congregating at home indoors. You could not possibly be positioned more poorly.”
Fauci, a leading member of the government’s coronavirus response, said the United States needed to make an “abrupt change” in public health practices and behaviors. He said the country could surpass 100,000 new coronavirus cases a day and predicted rising deaths in the coming weeks. He spoke as[ the nation set a new daily record Friday](https://www.washingtonpost.com/health/covid-deaths-increasing/2020/10/30/2269e88e-1a19-11eb-befb-8864259bd2d8_story.html?itid=lk_inline_manual_5) with more than 98,000 cases. As hospitalizations increase, deaths are also ticking up, with more than 1,000 reported Wednesday and Thursday, bringing the total to more than 230,000 since the start of the pandemic, according to health data analyzed by The Washington Post.
Fauci’s blunt warnings come as Trump has rallied in states and cities experiencing record surges in infections and hospitalizations in a last-ditch effort to convince voters he has successfully managed the pandemic. He has held maskless rallies with thousands of supporters, often in violation of local health mandates.
Even as new infections climb in 42 states, Trump has downplayed the virus or mocked those who take it seriously. “Covid-19, covid, covid, covid,” he said during one event, lamenting that the news media gives it too much attention. In another rally, he baselessly said that U.S. doctors record more deaths from covid-19, the disease the coronavirus causes, than other nations because they get more money.
“I mean our doctors are very smart people. So what they do is they say, ‘I’m sorry but everybody dies of covid,’ ” Trump said Friday at a rally in Waterford Township, Mich., without offering any evidence.
Trump Suggests He May Fire Fauci ‘After the Election’
The president’s comment further escalated the tension between his administration and Dr. Anthony S. Fauci, the nation’s top infectious disease expert, as coronavirus cases surge. Europe’s case count tops 10 million as lockdowns multiply.
President Trump suggested at a campaign rally early Monday morning that he might fire Dr. Anthony S. Fauci after Election Day, further escalating the tension between his administration and the nation’s top infectious disease expert as the number of new coronavirus cases in the United States reaches record highs.
Mr. Trump spoke well past midnight at the Miami-Opa Locka Executive Airport in Florida at his fifth and final rally of the day. At one point, he began reciting a familiar complaint about the news media’s continued coverage of the virus.
His grousing led the crowd of his supporters to begin chanting, “Fire Fauci! Fire Fauci!” Mr. Trump listened in silence for a few moments before remarking: “Don’t tell anybody, but let me wait until a little bit after the election. I appreciate the advice.”
The president’s aside came toward the end of what was a whirlwind day of campaigning across five states, and he spoke even as a local curfew aimed at curbing the spread of the coronavirus took effect at midnight. On Friday, more than 99,000 coronavirus infections were reported across the country, a single-day record. Nonetheless, Mr. Trump has maintained without citing evidence that the United States has “turned the corner” in fighting the virus, a point he reiterated at the rally early Monday.
That assertion is strongly disputed by Dr. Fauci, who told the The Washington Post in an interview published on Saturday that the United States “could not possibly be positioned more poorly” as it heads into winter. A White House spokesman later called Dr. Fauci’s comments “unacceptable.”
Former Vice President Joseph R. Biden Jr., the Democratic nominee, has said repeatedly that if he were to win the presidency, he is hopeful Dr. Fauci would remain in his role and serve in his administration.
States Undercount Positive Rapid Tests, Masking the Spread of Disease
As rapid coronavirus tests are becoming more widely available, delivering results in minutes for patients in doctor’s offices, nursing homes, schools and even the White House, officials warn of a significant undercount, blurring the virus’s spread nationally and in communities where such tests are more commonly used.
Public health officials say that antigen tests, which are faster than polymerase chain reaction (P.C.R.) tests but less able to detect low levels of the virus, are an important tool for limiting the spread of the coronavirus. But they caution that with inconsistent public reporting, the case undercount may worsen as more “point-of-care” antigen tests, as well as D.I.Y. and home test kits, come on the market.
“We want to be sure that we’re not now saying, ‘there’s no disease,’ when there is lots of disease. All that’s happened is that the science with which we identify it has evolved,” said Janet Hamilton, the executive director of the Council of State and Territorial Epidemiologists, the group that helps the Centers for Disease Control and Prevention define cases of the coronavirus.
Public health experts say that more coronavirus rapid testing will lead to more undercounting of coronavirus cases, even in states that attempt to count them publicly. What’s going on?
Some states do not count cases based on antigen tests
Despite C.D.C. guidance to report cases based on P.C.R. and antigen testing, Washington, D.C. and seven states don’t publicly share case counts for those with antigen positive tests, including California, New Jersey and Texas.
Another six states keep these tallies separate from their total case counts, and most of these report them less frequently.
Note: Data as of Oct. 29. Texas and Missouri publish antigen testing data but not cases. Local health agencies may report antigen cases in states where the health department does not.·Source: State health agencies
The differences among states are due in part to each state’s comfort level with the rapid tests, which aren’t “confirmatory” like P.C.R. tests because they can miss low levels of the virus. Yet most states treat antigen positive cases or “probable” cases the same as “confirmed” cases, by following up with interviews and contact tracing. And a growing number of states, including New Mexico, Oregon and Utah, include individuals with positive antigen tests in their total confirmed case counts.
Individuals who test positive from rapid tests are a small but growing share of all publicly reported cases. For example, in Florida, positive cases from antigen tests make up about 4 percent of all cases reported since March, the majority of which are based on P.C.R. But on a daily basis antigen tests contribute a more visible share, making up as much as a third of reported cases in recent days.
These counts are expected to increase as rapid tests purchased by the federal government reach schools and nursing homes across the country this fall.
And cases based on antigen tests can be even more significant in counties where these rapid tests have been more abundant.
For example, at least 26 of 254 Texas counties tally antigen positive cases on local health department websites, and several reveal an increasing dependence on rapid test results. The state health department doesn’t yet report these.
In Brown County, in west-central Texas, antigen tests have been widely available since the summer, so the county posts positive cases from rapid tests and from P.C.R. to offer a more complete view of infection, said Lisa Dick, administrator of the Brownwood-Brown County Health Department.
“If we just posted P.C.R. tests we would just be giving the community the idea that things were improving,” said Ms. Dick. “And people are making decisions based on that information, from leaders to individuals.”
In Taylor County in rural west Texas, individuals who test positive with rapid tests make up more than half of all cases, as the tests are accessible in the county’s many urgent care centers, said Dr. Annie Drachenberg, the medical director for Abilene-Taylor County Health District.
Patients also tend to prefer the same-day results that antigen tests offer, said Dr. Drachenberg, noting that the turnaround time for P.C.R. results peaked at two weeks over the summer before returning to one or two days this fall.
“Once you’ve broken that trust with a patient in terms of getting that answer quickly, it’s hard to get that trust back.”
Nontraditional testing centers can leave states in the dark
Whether states publicly report antigen positive cases or just track them internally, many public health officials say their counts are incomplete because they don’t know where rapid testing is taking place in their jurisdictions.
And unlike laboratories that typically perform more complicated P.C.R. tests, many of the “point-of-care” centers doing antigen testing, such as nursing homes, urgent care centers and schools, either don’t realize they need to report lab data, or may rely on slower, less efficient methods such as phone calls and faxes.
“We don’t know for sure what we don’t know,” said Dr. Edward Lifshitz, medical director of the Communicable Disease Service at the New Jersey Department of Health, which doesn’t publicly report antigen positive cases because the figure is incomplete.
Dr. Lifshitz added that sharing data on antigen positive cases might make some parts of the state, where point-of-care testing centers are reporting correctly, appear worse off than other areas that have missing data.
“It will look like, ‘boy, this part of the state is having an increase in cases,’ when it’s really not,” he said. “It’s just that they are reporting what they are supposed to be reporting.”
To avoid missing antigen test results, some health departments have had to do their own outreach.
In Houston, where infections surged over the summer, health officials searched for rapid testing centers online, made phone calls and posted a “dear provider” letter on their website. In New Jersey, officials have been collecting testing facility names from antigen test manufacturers and the Centers for Medicare and Medicaid Services, which distributed rapid tests to nursing homes across the state.
But even then, testing centers can still be missed.
Since late September, Alabama has reported three spikes of older cases because point-of-care facilities had neglected to report to public health officials their antigen test results. An urgent care group was responsible for the largest increase, which was reported on Oct. 23, after the addition of older cases nearly tripled the daily count.
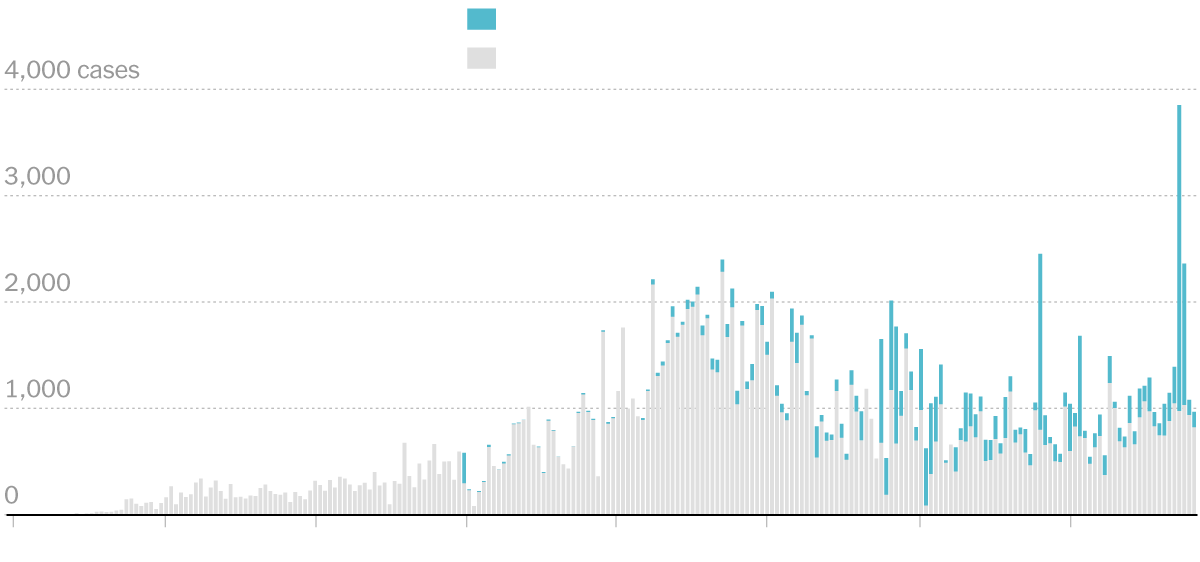
Daily reported new cases in Alabama
Alabama health officials say that as they learn of new testing centers, they are training them to share test data in an electronic format that they can easily work with. Health officials across the country in states like California, Georgia, New Jersey, Oklahoma and Texas, are doing the same, but training can be labor and time intensive, and many testing centers don’t have the technical support they need.
“This is a pipeline that is not well established,” said Kirstin Short, bureau chief of epidemiology at the Houston Health Department.
Many more tests are on the way
Scientists who follow the development of coronavirus tests say that rapid testing capacity — most of it antigen-based — could reach 200 million tests a month by early next year, and help the country reach recommended testing levels.
In September the country reported more than 20 million completed P.C.R. tests and about 5 million antigen tests, though the latter is a significant undercount, according to Mara G. Aspinall, a professor of practice in biomedical diagnostics at Arizona State University who tracks Covid-19 testing.
Antigen testing is also expected to grow beyond “point-of-care” tests to include portable kits that individuals can administer themselves. In fact, about two dozen companies are working on these personal rapid tests, according to Ms. Aspinall.
Public health officials say these home-based tests, much like a pregnancy test, may be nearly impossible to track. Some experts have also expressed concerns that home-based testing could come with its own set of pitfalls, as large groups of people inexperienced with administering tests use the products and try to interpret their results.
“We may eventually get these tests over the counter,” said Dr. Lifshitz of the New Jersey Department of Health. “From a public health perspective that’s a good thing. From a surveillance perspective that becomes a nightmare.”
Dr. Birx doing her best to warn the country about the ‘deadly phase’ of Covid.
**A top White House coronavirus adviser sounded alarms Monday about a new and **deadly phase in the health crisis, pleading with top administration officials for “much more aggressive action,” even as President Trump continues to assure rallygoers the nation is “rounding the turn” on the pandemic.
“We are entering the most concerning and most deadly phase of this pandemic … leading to increasing mortality,” said the Nov. 2 report from Deborah Birx, coordinator of the White House coronavirus task force. “This is not about lockdowns — It hasn’t been about lockdowns since March or April. It’s about an aggressive balanced approach that is not being implemented.”
Birx’s internal report, shared with top White House and agency officials, contradicts Trump on numerous points: While the president holds large campaign events with hundreds of attendees, most without masks, she explicitly warns against them. While the president blames rising cases on more testing, she says testing is “flat or declining” in many areas where cases are rising. And while Trump says the country is “rounding the turn,” Birx notes the country is entering its most dangerous period yet and will see more than 100,000 new cases a day this week.
In context: What Biden aide Ron Klain said about the swine flu
“It’s called the swine flu, right? And his own person, his chief of staff, said that he was — it was a disaster the way they ran it, a much less lethal problem, but a disaster the way they ran it, a total catastrophe. It was so bad, it was so bad.” — President Trump, remarks at a campaign rally , Oct. 12, 2020
“Joe Biden has no plan for Coronavirus — ALL TALK! He was a disaster in his handling of H1N1 Swine Flu. He didn’t have a clue, with his own Chief of Staff so saying.” — Trump, in a tweet , Oct. 8
These are just a couple of the many times that President Trump has referred to remarks by Ron Klain, a former chief of staff for Joe Biden, concerning the 2009-2010 swine flu pandemic. President Barack Obama is considered to have handled it pretty well, though that has not stopped Trump from arguing the opposite. An estimated 12,500 people died in the United States during that pandemic. (Here’s a fact check of Trump’s assertion about the swine flu pandemic.)
But there’s a video circulating with Klain’s remarks, and it sounds pretty damning. But, as always, we warn readers to ask: What is the context? Is there something missing?
Indeed, there is. Trump as usual overstates and twists what Klain said.
The Facts
We dug up the whole exchange on C-SPAN. The video above shows what Klain said immediately afterward. (We are limited to a 60-second clip off C-SPAN.) So here’s the context.
First, Klain in 2019 was appearing on a panel marking the 100th anniversary of the 1918 flu pandemic, hosted by the Scowcroft Institute of International Affairs. Much of the discussion is eerie in retrospect, as the participants note how unprepared the United States was if a similar viral event were to occur.
The specific question Klain was addressing, posed by moderator Andrew Natsios, director of the institute, was: “What could we do to create the incentives for industry to perhaps invest more money in research on this, for a universal flu vaccine, which, of course, companies are working on now?”
Klain had been the White House coordinator for responding to the Ebola outbreak in 2014-2015 but served as Biden’s chief of staff when the swine flu pandemic struck. This is the section that turns up in the videos on YouTube:
“I wasn’t involved directly in the H1N1 response, but I lived through it as a White House staffer. And what I will say about it is a bunch of really talented, really great people working on it. And we did every possible thing wrong. And it’s, you know, 60 million Americans got H1N1 in that period of time. And it’s just purely a fortuity that this isn’t one of the great mass casualty events in American history. Had nothing to do with us doing anything right. Just had to do with luck.”
But as Klain keeps going, he makes it clear he’s talking about vaccines.
“If anyone thinks this can’t happen again they don’t have to go back to 1918, they just have to go back to 2009-2010. Imagine a virus with a different lethality and you can just do the math on that. Now, what did that tell us? It told us that the vaccine will arrive late, told us that if it’s not prepared in advance or right away, if we don’t have the answer before, we’re not going to get the answer in time. And it told us that our systems for deciding how to distribute and administer vaccine in the time of crisis are going to be badly, badly tested. They also told us one other thing — that we really lack a global policy mechanism for dealing with these untested vaccines in an emergency situation.”
Indeed, there was an issue with developing the swine-flu vaccine during the outbreak. Not enough vaccines were produced, as the U.S. government decided to rely on a 50-year technology involving eggs — and the H1N1 virus grew more slowly in the eggs than expected.
“Even though the six-month goals for initial vaccine delivery were met, most of the vaccine arrived too late to vaccinate much of the public before the pandemic peaked,” the Health and Human Services Department concluded in a lengthy 2012 report, noting that early projections “regarding timing of vaccine supply changed frequently and were inaccurate. This led to public confusion and temporary erosion of confidence in the federal government, and created challenges for the planning and execution of local vaccine administration efforts.”
But, in what the report called “serendipity,” it turned out that just one dose was effective, rather than the anticipated two, so the supply that was produced went twice as far. Because that flu turned out to be relatively mild, hospitals were not as stressed as might have been expected.
That’s what Klain meant when he referred to luck.
“The point I was trying to make was about an over reliance on vaccines as a single strategy for coping with pandemics,” Klain told The Fact Checker in an email. “That was not in fact what happened on H1N1 but there had been a lot of chatter at the conference I was attending about vaccines as the dominant strategy.
“What I was trying to say was that if one relies only on vaccines as your major strategy, and vaccines are late then you are screwed, and really bad things can happen,” Klain added. “Of course H1N1 was beaten without much use of the vaccine. Of course, you could argue that what Trump has been doing the past few months — downplaying testing, downplaying masks, downplaying tracing and other public health measures, while promising a cure/vaccine is ‘just around the corner’ — proves my point: The U.S. death rate from covid post-June is unmatched in the world.”
Indeed, when the Scowcroft Institute issued a news release on the conference, it used Klain’s quote to highlight that the United States was not prepared for a possible pandemic:
During the final panel of the afternoon, Ron Klain, who served as the White House Ebola Response Coordinator from 2014 to 2015 and as Chief of Staff to Vice Presidents Al Gore and Joe Biden, urged attendees to not take the current pandemic response infrastructure for granted and to keep striving for improvements.
He recalled the 2009-2010 H1N1 flu pandemic, which recorded an estimated 60 million cases and 12,000 deaths, as an example.
“It’s purely a fortuity that this wasn’t one of the great mass casualty events in American history,” Klain said. "It had nothing to do with us doing anything right, it just had to do with luck. If anyone thinks this can’t happen again they don’t have to go back to 1918, they just have to go back to 2009-2010.”
The Bottom Line
Video is a powerful medium, but readers must be wary about whether they understand the full context of the clip they are watching. Judging from our emails, many readers have been tricked by video snippets that the Trump campaign has used regarding fracking, funding of police and Biden’s role in Ukraine. We have not seen this particular clip used in any Trump TV ads, but Trump frequently mischaracterizes Klain’s point. It’s clear he was not talking about the overall response to the swine-flu pandemic or Biden’s role in it. Instead, he was making a point that in retrospect was rather prescient.
5 things states must do to curb the spread of COVID-19: ANALYSIS

Gods. If things stay at this rate, we’ll soon be having over 1 MILLION new cases a WEEK. In fact, it might be THIS week, and definitely will be NEXT week if this number doesn’t drop precipitously.
‘We’re not going to control the pandemic.’ Mark Meadows