The final legacy of the former guy: a never-ending cycle of vaccines and outbreaks because of his botched response and outright lies and selfishness.
Reaching ‘Herd Immunity’ Is Unlikely in the U.S., Experts Now Believe
Widely circulating coronavirus variants and persistent hesitancy about vaccines will keep the goal out of reach. The virus is here to stay, but vaccinating the most vulnerable may be enough to restore normalcy.
Early in the pandemic, when vaccines for the coronavirus were still just a glimmer on the horizon, the term “herd immunity” came to signify the endgame: the point when enough Americans would be protected from the virus so we could be rid of the pathogen and reclaim our lives.
Now, more than half of adults in the United States have been inoculated with at least one dose of a vaccine. But daily vaccination rates are slipping, and there is widespread consensus among scientists and public health experts that the herd immunity threshold is not attainable — at least not in the foreseeable future, and perhaps not ever.
Instead, they are coming to the conclusion that rather than making a long-promised exit, the virus will most likely become a manageable threat that will continue to circulate in the United States for years to come, still causing hospitalizations and deaths but in much smaller numbers.
How much smaller is uncertain and depends in part on how much of the nation, and the world, becomes vaccinated and how the coronavirus evolves. It is already clear, however, that the virus is changing too quickly, new variants are spreading too easily and vaccination is proceeding too slowly for herd immunity to be within reach anytime soon.
Continued immunizations, especially for people at highest risk because of age, exposure or health status, will be crucial to limiting the severity of outbreaks, if not their frequency, experts believe.
“The virus is unlikely to go away,” said Rustom Antia, an evolutionary biologist at Emory University in Atlanta. “But we want to do all we can to check that it’s likely to become a mild infection.”
The shift in outlook presents a new challenge for public health authorities. The drive for herd immunity — by the summer, some experts once thought possible — captured the imagination of large segments of the public. To say the goal will not be attained adds another “why bother” to the list of reasons that vaccine skeptics use to avoid being inoculated.
Yet vaccinations remain the key to transforming the virus into a controllable threat, experts said.
Dr. Anthony S. Fauci, the Biden administration’s top adviser on Covid-19, acknowledged the shift in experts’ thinking.
“People were getting confused and thinking you’re never going to get the infections down until you reach this mystical level of herd immunity, whatever that number is,” he said.
“That’s why we stopped using herd immunity in the classic sense,” he added. “I’m saying: Forget that for a second. You vaccinate enough people, the infections are going to go down.”
Why reaching the threshold is tough
Once the novel coronavirus began to spread across the globe in early 2020, it became increasingly clear that the only way out of the pandemic would be for so many people to gain immunity — whether through natural infection or vaccination — that the virus would run out of people to infect. The concept of reaching herd immunity became the implicit goal in many countries, including the United States.
Early on, the target herd immunity threshold was estimated to be about 60 to 70 percent of the population. Most experts, including Dr. Fauci, expected that the United States would be able to reach it once vaccines were available.
But as vaccines were developed and distribution ramped up through the winter and into the spring, estimates of the threshold began to rise. That is because the initial calculations were based on the contagiousness of the original version of the virus. The predominant variant now circulating in the United States, called B.1.1.7 and first identified in Britain, is about 60 percent more transmissible.
As a result, experts now calculate the herd immunity threshold to be at least 80 percent. If even more contagious variants develop, or if scientists find that immunized people can still transmit the virus, the calculation will have to be revised upward again.
Polls show that about 30 percent of the U.S. population is still reluctant to be vaccinated. That number is expected to improve but probably not enough. “It is theoretically possible that we could get to about 90 percent vaccination coverage, but not super likely, I would say,” said Marc Lipsitch, an epidemiologist at the Harvard T.H. Chan School of Public Health.
Though resistance to the vaccines is a main reason the United States is unlikely to reach herd immunity, it is not the only one.
Herd immunity is often described as a national target. But that is a hazy concept in a country this large.
“Disease transmission is local,” Dr. Lipsitch noted.
“If the coverage is 95 percent in the United States as a whole, but 70 percent in some small town, the virus doesn’t care,” he explained. “It will make its way around the small town.”
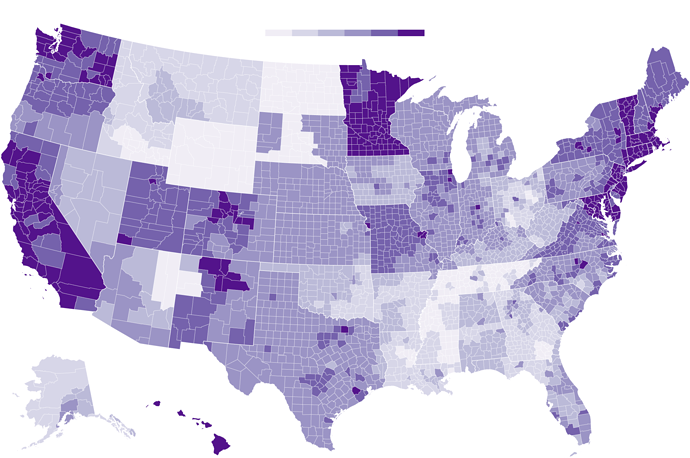
Uneven Willingness to Get Vaccinated Could Affect Herd Immunity
In some parts of the United States, inoculation rates may not reach the threshold needed to prevent the coronavirus from spreading easily.
How insulated a particular region is from the coronavirus depends on a dizzying array of factors.
Herd immunity can fluctuate with “population crowding, human behavior, sanitation and all sorts of other things,” said Dr. David M. Morens, a virologist and senior adviser to Dr. Fauci. “The herd immunity for a wealthy neighborhood might be X, then you go into a crowded neighborhood one block away and it’s 10X.”
Given the degree of movement among regions, a small virus wave in a region with a low vaccination level can easily spill over into an area where a majority of the population is protected.
At the same time, the connectivity between countries, particularly as travel restrictions ease, emphasizes the urgency of protecting not just Americans but everyone in the world, said Natalie E. Dean, a biostatistician at the University of Florida in Gainesville. Any variants that arise in the world will eventually reach the United States, she noted.
Many parts of the world lag far behind the United States on vaccinations. Less than 2 percent of the people in India have been fully vaccinated, for example, and less than 1 percent in South Africa, according to data compiled by The New York Times.
“We will not achieve herd immunity as a country or a state or even as a city until we have enough immunity in the population as a whole,” said Lauren Ancel Meyers, the director of the Covid-19 Modeling Consortium at the University of Texas at Austin.
What the future may hold
If the herd immunity threshold is not attainable, what matters most is the rate of hospitalizations and deaths after pandemic restrictions are relaxed, experts believe.
By focusing on vaccinating the most vulnerable, the United States has already brought those numbers down sharply. If the vaccination levels of that group continue to rise, the expectation is that over time the coronavirus may become seasonal, like the flu, and affect mostly the young and healthy.
“What we want to do at the very least is get to a point where we have just really sporadic little flare-ups,” said Carl Bergstrom, an evolutionary biologist at the University of Washington in Seattle. “That would be a very sensible target in this country where we have an excellent vaccine and the ability to deliver it.”
Over the long term — a generation or two — the goal is to transition the new coronavirus to become more like its cousins that cause common colds. That would mean the first infection is early in childhood, and subsequent infections are mild because of partial protection, even if immunity wanes.
Some unknown proportion of people with mild cases may go on to experience debilitating symptoms for weeks or months — a syndrome called “long Covid” — but they are unlikely to overwhelm the health care system.
“The vast majority of the mortality and of the stress on the health care system comes from people with a few particular conditions, and especially people who are over 60,” Dr. Lipsitch said. “If we can protect those people against severe illness and death, then we will have turned Covid from a society disrupter to a regular infectious disease.”
If communities maintain vigilant testing and tracking, it may be possible to bring the number of new cases so low that health officials can identify any new introduction of the virus and immediately stifle a potential outbreak, said Bary Pradelski, an economist at the National Center for Scientific Research in Grenoble, France. He and his colleagues described this strategy in a paper published on Thursday in the scientific journal The Lancet.
“Eradication is, I think, impossible at this stage,” Dr. Pradelski said. “But you want local elimination.”
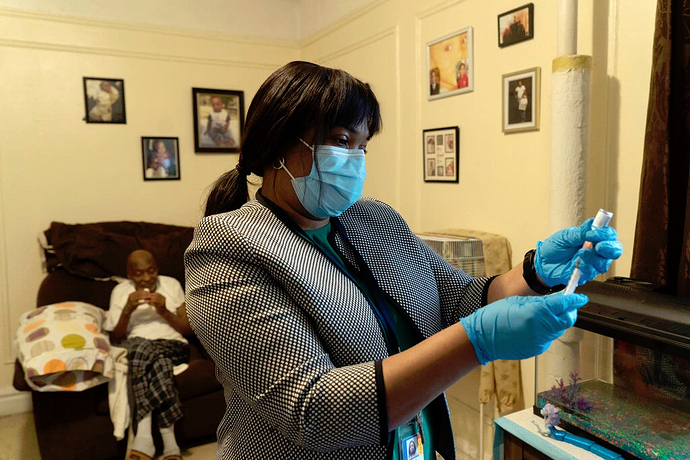
Darcia Bryden-Currie, a nurse, preparing a vaccine for Stephen Elliot at his home in the Bronx, part of an inoculation program for homebound people.
Vaccination is still the key
The endpoint has changed, but the most pressing challenge remains the same: persuading as many people as possible to get the shot.
Reaching a high level of immunity in the population “is not like winning a race,” Dr. Lipsitch said. “You have to then feed it. You have to keep vaccinating to stay above that threshold.”
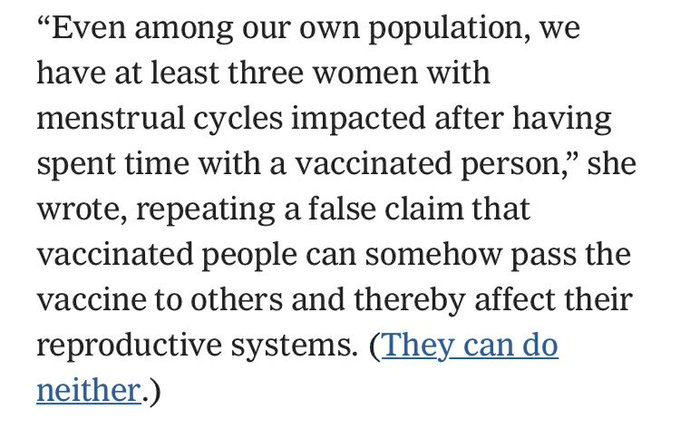
Skepticism about the vaccines among many Americans and lack of access in some groups — homeless populations, migrant workers or some communities of color — make it a challenge to achieve that goal. Vaccine mandates would only make that stance worse, some experts believe.
A better approach would be for a trusted figure to address the root cause of the hesitancy — fear, mistrust, misconceptions, ease of access or a desire for more information, said Mary Politi, an expert in health decision making and health communication at Washington University in St. Louis.
People often need to see others in their social circle embracing something before they are willing to try it, Dr. Politi said. Emphasizing the benefits of vaccination to their lives, like seeing a family member or sending their children to school, might be more motivating than the nebulous idea of herd immunity.
“That would resonate with people more than this somewhat elusive concept that experts are still trying to figure out,” she added.
Though children spread the virus less efficiently than adults do, the experts all agreed that vaccinating children would also be important for keeping the number of Covid cases low. In the long term, the public health system will also need to account for babies, and for children and adults who age into a group with higher risk.
Unnerving scenarios remain on the path to this long-term vision.
Over time, if not enough people are protected, highly contagious variants may develop that can break through vaccine protection, land people in the hospital and put them at risk of death.
“That’s the nightmare scenario,” said Jeffrey Shaman, an epidemiologist at Columbia University.
How frequent and how severe those breakthrough infections are have the potential to determine whether the United States can keep hospitalizations and deaths low or if the country will find itself in a “mad scramble” every couple of years, he said.
“I think we’re going to be looking over our shoulders — or at least public health officials and infectious disease epidemiologists are going to be looking over their shoulders going: ‘All right, the variants out there — what are they doing? What are they capable of?” he said. “Maybe the general public can go back to not worrying about it so much, but we will have to.”