It would appear that Putin’s mask has fallen.
This is what you call checkmate.
‘We’re beyond angered’: Fed-up nurses file lawsuits, plan protest at White House over lack of coronavirus protections
For Pamella Brown-Richardson, a nurse practitioner in New York, the fever and cough came in mid-March. Soon after, her fever worsened, and she began experiencing shortness of breath and body aches — telltale symptoms of the novel coronavirus. By early April, Brown-Richardson was in the emergency room with double-lobe pneumonia caused by covid-19.
As Brown-Richardson tells it, there is probably only one place where she could have been exposed to the virus: the primary care clinic in the Bronx, where she says she spent days caring for people suffering from covid-19 symptoms with just a flimsy surgical mask as protection.
Brown-Richardson is one of more than a dozen nurses in New York, the epicenter of the U.S. coronavirus outbreak, who detailed their experiences on the front lines in affidavits corroborating three lawsuits filed Monday against the state health department and two area hospitals. The complaints, which were lodged by New York’s largest nurses union, allege that inadequate protective equipment, among other failures, contributed to “compromising the health and safety of the nurses,” according to a news release from the union.
“These lawsuits were filed to protect our nurses, our patients and our communities from grossly inadequate and negligent protections,” Pat Kane, executive director of the New York State Nurses Association, said in the release. “We cannot allow these dangerous practices to continue.”
More than 9,000 health-care workers in the United States have tested positive for the novel virus, according to recent figures from the Centers for Disease Control and Prevention. But as The Washington Post’s Ariana Eunjung Cha reported, the numbers are “believed to be a gross undercount of infections due to the continuing lack of available tests in many areas,” with some regions and facilities choosing not to test health-care workers in favor of saving kits for their sickest patients.
Among nurses, frustration over being forced to choose between doing their jobs and risking exposure to a potentially deadly virus appears to be reaching a tipping point this week. Beyond taking legal action, as in the case of New York’s caregivers, members of National Nurses United, the country’s largest union of registered nurses, have planned a protest outside the White House on Tuesday morning to raise awareness of their plight and demand federal funding for the mass production of personal protective equipment.
“We’re tired of being treated as if we are expendable,” Deborah Burger, president of National Nurses United, which has more than 150,000 members, told The Post. “If we are killed in this pandemic, there won’t be anybody to take care of the rest of the sick people that are going to come.”
She later added, “We’re beyond angered at this.”
Press Release: Nurses to Protest at White House to Demand OSHA Standard and Mass Production of PPE for Health Care Workers
Nurses demand Congress include a mandatory OSHA emergency standard in its next #COVID19 legislative package.https://bit.ly/2xB5FaP #ProtectNurses pic.twitter.com/VoCT4X0IGB
— NationalNursesUnited (@NationalNurses) April 20, 2020
At Tuesday’s protest, the names of nurses who have died of covid-19 in the United States will be read out loud, according to a news release. While there aren’t official statistics available on the number of nurses who contracted fatal infections, Burger said she estimates that the count exceeds more than a hundred.
Many, if not all, of the cases involving health-care workers could have been prevented had sufficient safeguards been in place, she said.
“Everybody says they love nurses, they want to protect us, but we still don’t have the safety gear that we need,” said Burger, who has been a registered nurse for more than 45 years.
As detailed in the lawsuits filed in New York, nurses there allege that the virus’s spread was aided in part by a lack of proper safety supplies. The complaints named the New York State Department of Health and two hospitals, Montefiore Medical Center and Westchester Medical Center, as defendants.
Several nurses alleged that they were told to use one N95 mask per week and were given paper bags in which to store their masks and no sanitation instructions, according to court documents. Others, like Brown-Richardson, say they were not provided with certain protective equipment despite numerous requests.
“We were instructed that we could only wear a surgical mask, which is not adequate protection against COVID-19, if the patient presented with a cough,” Brown-Richardson wrote in her affidavit. “Otherwise we were prohibited from wearing a surgical mask because management believed that doing so could alarm patients.”
The lawsuits also claimed that nurses and other health-care workers presenting covid-19 symptoms have been denied testing, raising the risk that they might unknowingly transmit the disease to their loved ones or anyone else with whom they may come in contact.
A spokesperson for the state health department told The Post in a statement that it cannot comment on pending litigation. But the spokesperson stressed that the department is “deeply grateful for the ongoing efforts of New York’s health care workers to reduce the spread of COVID-19 by testing people who may be infected and treating those who are most in need.”
“The State of New York continues to take every step necessary to ensure that health care workers, particularly those who are sampling and providing direct care, have the support and supplies needed to address this unprecedented public health emergency,” the statement said.
The Westchester Medical Center Health Network disputed the lawsuit’s claims.
“While we cannot comment on pending litigation, we know, and our care providers know, that the allegations in NYSNA’s lawsuit are wrong,” the network said in an emailed statement. “Our focus is, and has always been, protecting our workforce, which has been aligned from the outset in treating the most severely ill patients battling COVID-19.”
In a statement to The Post, the Montefiore Medical Center said the New York nursing union’s leadership “has chosen to attack a system, and the commitment of thousands of their colleagues, who have followed the Governor’s emergency orders and are selflessly doing all they can to fight COVID-19 and save lives.”
Meanwhile, Burger said the ability to bring change lies in the hands of the Trump administration and Congress. In addition to seeking federal funding, National Nurses United is calling on President Trump to use the Defense Production Act to produce supplies such as protective gear and testing kits, according to the news release. In recent weeks, Trump has used the act to increase the production of ventilators and other medical equipment, The Post reported.
Still, Burger said the protections currently being provided to health-care workers are not nearly enough.
“Every time I talk to nurses, it’s like they have never felt so disrespected and ignored,” she said. “They give firemen what they need to go into a burning building. They give policemen bulletproof vests and guns and Tasers and tear gas. What do we get? A bandanna or a scarf.”
These Photos Show the Staggering Food Bank Lines Across America
America’s hunger is being captured by photographers across the country.
Trump Administration Slow to Distribute Coronavirus Aid to Hospitals
“We approved the $100 billion and only $30 billion has gone out,” said Sen. John Barrasso (R., Wyo.), who has been speaking with HHS Secretary Alex Azar. Mr. Barrasso said he had expected more funding to have been disbursed by now. None of the remaining $70 billion is expected to be distributed this week, according to two people familiar with the planning.
Trump move to end WHO funding would be ‘catastrophic’ for polio programs, experts warn
Covid-19 is rapidly becoming America’s leading cause of death
How does the coronavirus compare to other major causes of death in an average week?
February 6th!
Watch Vegas Mayor Advocate Survival of the Fittest Reopening Strategy, With Total Disregard for Human Life
“Well, we’ll find out the facts after [we reopen the city]. Unfortunately, we all do better in hindsight,” Mayor Carolyn Goodman said
At least two people who died in early and mid-February had contracted the novel coronavirus, health officials in California said Tuesday, signaling the virus may have spread — and been fatal — in the United States weeks earlier than previously thought.
https://www.washingtonpost.com/nation/2020/04/22/death-coronavirus-first-california/
US is far from flattening the curve. Check out all the most recent data compiled here.
Billionaire shipping magnate & Trump mega-donor Liz Uihlein sent email to her employees urging them to support a recall of Democratic Wisconsin Gov. Tony Evers for “violating their constitutional right to work” during the pandemic.
More astroturfing.
https://www.bloomberg.com/news/articles/2020-04-21/trump-mega-donor-a-shipping-magnate-pushes-to-end-a-shutdown
McConnell says no ‘blue state’ coronavirus bailouts, effectively telling New York to drop dead
Stimulus Proposal: $2,000 Payment Plus $1,000 Per Month Until 1 Year After Crisis Ends
Gilead Sciences Inc’s experimental coronavirus drug failed its first randomised clinical trial, the Financial Times reported on Thursday, citing draft documents published accidentally by the World Health Organization.
Trading in the shares of the company was halted after they fell 6%.
The Chinese trial showed the antiviral remdesivir did not improve patients’ condition or reduce the pathogen’s presence in the bloodstream, the report https://on.ft.com/2VumJIA said.
Glad that Obama is weighing in on the lack of a “coherent national plan.” He’s getting more involved in shining a light on how ineffective T has been. Thank you.
Former President Obama on Wednesday called out the Trump administration’s failure to form a “coherent national plan” as it navigates the outbreak of COVID-19, the disease caused by the novel coronavirus.
The former president hailed states that are developing their own strategies despite a unified plan, specifically citing Massachusetts’s statewide effort.
“While we continue to wait for a coherent national plan to navigate this pandemic, states like Massachusetts are beginning to adopt their own public health plans to combat this virus––before it’s too late,” Obama said on Twitter, linking to a New Yorker article that details Gov. Charlie Baker’s ® aggressive push for widespread testing and a comprehensive contact-tracing program.
While we continue to wait for a coherent national plan to navigate this pandemic, states like Massachusetts are beginning to adopt their own public health plans to combat this virus––before it’s too late. https://www.newyorker.com/science/medical-dispatch/its-not-too-late-to-go-on-offense-against-the-coronavirus
Barack Obama (@BarackObama) April 22, 2020**
Obama rarely weighs in on policies or plans developed by the current administration. But he has remained vocal on Twitter and other platforms during the coronavirus outbreak. In late March, he urged local governments around the nation to maintain social-distancing requirements as some lawmakers began pushing for reopening portions of the economy.
“Tide Pods” is trending because Trump does not understand when people are humoring him because he is saying STUPID F$%KING THINGS but is also the president and their boss.
No, we can’t inject UV light, bleach, or alcohol to kill the coronavirus.
Read the comments in response. Seriously.
“Former President Obama on Wednesday called out the Trump administration’s failure to form a “coherent national plan” as it navigates the outbreak of COVID-19, the disease caused by the novel coronavirus.”
“A coherent national plan?” But…that’s IMPOSSIBLE, especially when there’s an unproven drug that might kill you but our president has a financial interest in.
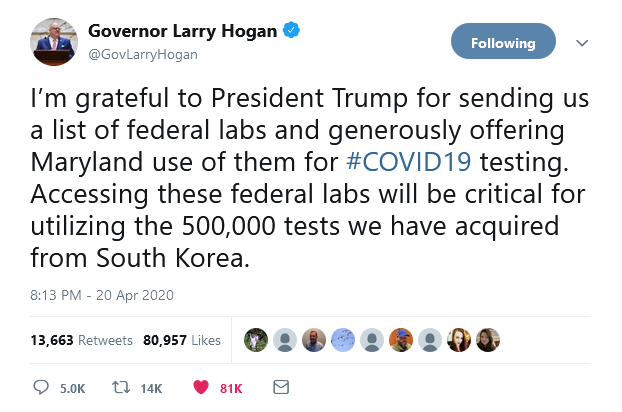
Oh wait…there’s South Korea, with a not just coherent national plan, but an organized, coordinated, and properly executed national plan that’s actually WORKING. We could do THAT, right? Nah…We’re the United States of Donald Trump.
And just think what’s going to happen when the Stay @Home orders are rescinded and everyone’s sent back out again, with no other changes made. But we’ve no way of knowing what’s going to happen, right? So we might as well just TRY it!
Oh wait…that’s what they did in China, right? And what happened? The curve started back UP again. Are we REALLY this STUPID?
Some really good insights into where we are with the Pandemic by Bill Gates, and suggesting that we are in Pandemic I with a potential 5 years until we find an effective vaccine.
You can download it into a PDF (red link)
The coronavirus pandemic pits all of humanity against the virus. The damage to health, wealth, and well-being has already been enormous. This is like a world war, except in this case, we’re all on the same side. Everyone can work together to learn about the disease and develop tools to fight it. I see global innovation as the key to limiting the damage. This includes innovations in testing, treatments, vaccines, and policies to limit the spread while minimizing the damage to economies and well-being.
This memo shares my view of the situation and how we can accelerate these innovations. (Because this post is long, it is also available as a PDF.) The situation changes every day, there is a lot of information available—much of it contradictory—and it can be hard to make sense of all the proposals and ideas you may hear about. It can also sound like we have all the scientific advances needed to re-open the economy, but in fact we do not. Although some of what’s below gets fairly technical, I hope it helps people make sense of what is happening, understand the innovations we still need, and make informed decisions about dealing with the pandemic.
Exponential growth and decline
In the first phase of the pandemic, we saw an exponential spread in a number of countries, starting with China and then throughout Asia, Europe, and the United States. The number of infections was doubling many times every month. If people’s behavior had not changed, then most of the population would have been infected. By changing behavior, many countries have gotten the infection rate to plateau and start to come down.
Exponential growth is not intuitive. If you say that 2 percent of the population is infected and this will double every eight days, most people won’t immediately figure out that in 40 days, the majority of the population will be infected. The big benefit of the behavior change is to reduce the infection rate dramatically so that, instead of doubling every eight days, it goes down every eight days.
We use something called the reproduction rate, or R0 (pronounced “are-nought”), to calculate how many new infections are caused by an earlier infection. R0 is hard to measure, but we know it’s below 1.0 wherever the number of cases is going down and above 1.0 wherever the number of cases is going up. And what may appear to be a small difference in R0 can lead to very large changes.
If every infection goes from causing 2.0 cases to only causing 0.7 infections, then after 40 days you have one-sixth as many infections instead of 32 times as many. That’s 192 times fewer cases. Here’s another way to think about it: If you started with 100 infections in a community, after 40 days you would end up with 17 infections at the lower R0 and 3,200 at the higher one. Experts are debating now just how long to keep R0 very low to drive down the number of cases before opening up begins.
Exponential decline is even less intuitive. A lot of people will be stunned that in many places we will go from hospitals being overloaded in April to having lots of empty beds in July. The whiplash will be confusing, but it is inevitable from the exponential nature of infection.
As we get into the summer, some locations that maintain behavior change will experience exponential decline. However, as behavior goes back to normal, some locations will stutter along with persistent clusters of infections and some will go back into exponential growth. The picture will be more complex than it is today, with a lot of heterogeneity.
Special Report: As virus advances, doctors rethink rush to ventilate
FFS
Is the official COVID-19 death count too low? Funeral directors, EMS workers say yes
We’re fixated on the official data, which is bad enough. But we may be missing a bigger and more lethal picture
We are now well into the second month of the COVID-19 crisis, which has been largely framed, in the New York region, by Gov. Andrew Cuomo’s and Gov. Phil Murphy’s daily briefings and daily data dumps, which include hospitalizations, the number of intensive care unit patients, intubations, patient discharges and confirmed cases.
Based on the arc of those data points, both Cuomo and Murphy have sounded guardedly optimistic in recent days that the public’s compliance with social distancing and stay-at-home orders are producing the desired effect of reducing the crush of demand on the health care system. Deaths and hospitalizations in both New York and New Jersey appear to be decreasing.
George Kelder is CEO and executive director of the New Jersey State Funeral Directors Association, whose members are responsible for dealing with bodies at the hospital, congregant care facilities and private residences. He warns that if we rely solely on official numbers carried on the TV, we may not fully appreciate the lethality of the virus, and indeed may overestimate our success in combating it.
In a phone interview, Kelder confirmed that on April 15 New Jersey’s Office of Vital Statistics and Registry, in accordance with the CDC’s National Vital Statistics System, had ordered that deaths of confirmed or suspected COVID-19 patients should no longer be reported with that disease as the immediate cause of death.
“The guidance, available on the New Jersey’s Electronic Death Registration System website, states that COVID-19 is not considered an immediate cause of death and should NOT be reported by the medical certifier on the first line of section 36a (CAUSE OF DEATH, PART I) of the death certificate,” the association advised its members. “Instead, the immediate cause of death, such as “Acute Respiratory Distress Syndrome,” should be listed on the first line. COVID-19 should be listed LAST in Section 36a after the immediate cause(s) has been listed.”
“During the five weeks of these fatalities, New Jersey physicians had been instructed to used COVID-19, Coronavirus 19 or ‘pending COVID-19’ as the primary cause of death,” Kelder said. “Last week, because of changes on the national level, the primary cause of death can no longer be COVID-19. It can be a secondary cause or a consequence of the primary cause of death. But the primary cause of death must be something other than the virus itself.”
Kelder observed that pervasive lack of testing, along with this bureaucratic gamesmanship around how COVID-19 deaths are to be classified, could mean that the numbers being used officially "would not be equal to what is happening on the street.
“My concern is that we will be getting a false sense of the fatalities based on an administrative and statistical change in reporting,” he said.
Lost in the abstraction of the daily graphs that track a the state’s “progress” is the actual scale of the number of deaths and how the volume is overwhelming the funeral industry itself.
Bob Prout is a third-generation funeral director who runs his environmentally-minded funeral home in Verona, New Jersey, with his daughter Julia. They have been dealing with the full gamut of COVID-19 confirmed and suspected cases in hospitals, congregant living and residential settings.
“Most people are having a hard time with the sheer volume of deaths and realizing that when a burial happens it is out of the funeral parlor’s hands,” he said during a phone interview. "Even if a family has set aside a burial plot, cemeteries have such a huge volume and a backlog.
“Even our state’s crematoriums are backed up as much as three weeks because the New York funeral directors are sending their bodies over here,” Prout continued. “I wish the governor would sign an executive order that for 60 or 90 days our state’s crematoriums would have to handle just the bodies of New Jersey residents who lived and paid taxes here.”
Kelder opposes such a restriction, saying it could end reciprocal arrangements between New York, Pennsylvania and New Jersey that make it possible for families in one of those states to bury a loved one in another.
The Prouts say they now consider that any body they encounter, no matter the location or circumstances, is a possible COVID-19 case. They take universal precautions based on the latest guidelines from their national trade association that tracks the CDC guidelines.
Personal protective equipment has also been a problem for the funeral industry. “We are at a critical stage on this and are looking to the New Jersey State Police to unlock the supply chain,” said Kelder. “When we look back at this it will be clear we have not factored in mortuary care as part of the health care system.”
Kelder says the greatest threat to the health of his members and their employees comes from surviving family members of a COVID-19 virus fatality who were likely exposed to that person when he or she was still alive, and are now infected with no symptoms. “We have surviving family members who think it is OK to break their quarantine to deal with the final arrangements for their loved ones,” he said.
On April 14, even before the changes to the way COVID-19 deaths are recorded, Newark Patch reported that officials in densely populated Essex County had conceded that the actual number of the deaths due to the pandemic were “much greater than indicated.”
Throughout the crisis it’s been the deaths in hospitals and senior citizens facilities that are counted and widely reported, whereas the elevated number of deaths at home received scant attention.
In an April 18 phone interview, the Rev. Tony Johnson and Jody Leight, who live in Orange, New Jersey, described seeing local EMTs respond to a neighbor’s home wearing biohazard protective gear, while a police patrol car stayed parked outside. Their neighbor’s body was retrieved from the residence five hours later.
Leight explained that their community has many undocumented immigrants “who are out there working jobs where they have no protective equipment. They are working jobs off the books and living four or five families to one house. How is social distancing even possible?” Orange has no hospital, she continued. “I am concerned we have hundreds of people here who are at risk and will most likely die in their homes.”
At one point earlier this month, the FDNY confirmed that over several days New York City was averaging well over 200 residential fatal heart attacks a day, a tenfold increase over the number recorded this time last year. As recently as this past weekend, the number of cardiac arrests were running exponentially higher than would normally be recorded this time of year.
In subsequent conversations with leaders of the EMS unions, I have been told that their members were encountering people who had actually been released from the hospital only to die at home, and others who had delayed seeking medical attention for fear of being taken to a hospital and exposed to COVID-19.
Dr. Joseph Fennelly, an internist who served for decades as the chairman or co-chairman of the Medical Society of New Jersey’s bioethics committee, thinks that the fight to contain COVID-19 can’t be just limited to the hospitals and congregant care facilities that have generated the headlines. The virus, he says, is not just inside these facilities but in the community.
“You have to look at this in terms of a cell, a living system, and what the energy is that feeds it,” he said. “You can’t get a handle on that without looking at the residential facet of this.”
One way to do that in real time, Fennelly posits, would be to track deaths at home in real time, even if they can’t be conclusively linked to COVID-19, as a way of getting a bead on what we don’t know.
Certainly, we should at least learn how many of those deaths at home were people who had already been discharged by hospitals. It would certainly put those patient discharge numbers, on which both Murphy and Cuomo rely so heavily, in their proper context.