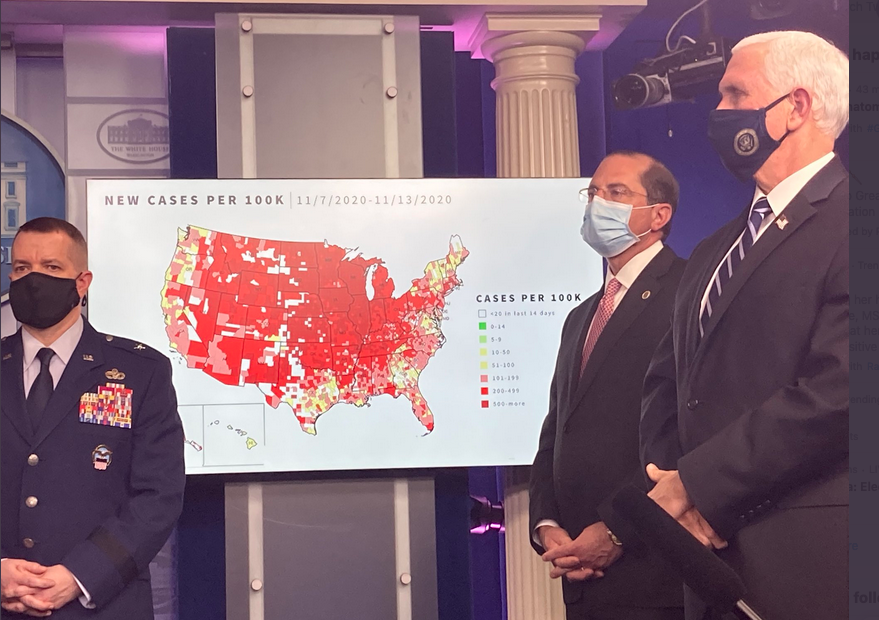
We are facing unprecedented amount of Covid infections, and once Biden takes power, the increasing numbers seem beyond daunting. Some strategies that they might employ involve getting help from the Right - former Senator Dr. Frist who is also a doctor, and a Republican to set up a straight narrative (from that Right.) Perhaps they might also get Hannity or Carlson’s help, but someone like Lebron James may be able to help as well.
Long, well-researched article in NYT…on where we are with the pandemic, how to plan for large numbers, what the vaccine can do and where Biden must act.
Mr. Biden has said he supports a national mask mandate, although his plan calls on governors to impose state ones.
Among the suggested names with those skills were Heidi J. Larson of the Vaccine Confidence Project in London, Carl T. Bergstrom of the University of Washington and Zeynep Tufekci of the University of North Carolina.
Others said the panel had too many members tied to the Obama-Biden administration. Dr. Ezekiel J. Emanuel, for example, was an architect of the Affordable Care Act and Dr. Eric Goosby was Mr. Obama’s global AIDS coordinator. To reach Mr. Trump’s base, they said, the panel needs credible Republican experts.
“Otherwise,” said Dr. Leana Wen, a former Baltimore health commissioner, “there will be even more of a mistaken perception that this is Democrats and doctors trying to shut down the economy, when actually controlling the virus is key to economic recovery.”
Experts suggested adding Dr. Bill Frist, a transplant surgeon and former Republican senator, or Dr. Marc K. Siegel, an internist and Fox News opinion writer.
Mr. Warren suggested consulting marketing experts and recruiting “everyone from Santa Claus to LeBron James” as trusted spokesmen.
Another expert suggested adding Dr. Mehmet C. Oz, a heart surgeon and television personality who was criticized for promoting hydroxychloroquine on Fox News (he later relented), and possibly even asking Sean Hannity and Tucker Carlson to join, because they are popular with Mr. Trump’s base and might be persuaded to accept science that would save the lives of their own viewers.
…
All the experts interviewed by The Times praised the plan, but several felt it was not aggressive enough. The pandemic is raging so far beyond control, they argued, that it can be contained only with deeply unpopular but necessary measures, such as rigorously enforced mask laws, closing bars and restaurants, requiring regular testing in schools and workplaces, isolating the infected away from their families, prohibiting travel from high-prevalence areas to low ones, and imposing quarantines that are enforced rather than merely requested.
Many other countries have imposed such measures despite fierce opposition from some citizens, they said, and they have helped.
“Colleges are the Wuhans of this fall surge,” said Dr. Howard Markel, a medical historian at the University of Michigan’s medical school. Universities, he and other experts said, must stop students from going back and forth between their hometowns and college towns, both of which have many vulnerable residents.
…
The next dozen weeks will be long and painful. But spring is likely to bring highly effective vaccines and a renewed commitment to medical leadership, something that has been missing under Mr. Trump.
“The C.D.C. will have to be rebuilt, and its guidelines and the F.D.A.’s have to be promptly re-evaluated,” said Dr. Robert L. Murphy, director of the Institute for Global Health at Northwestern University’s medical school. “The Biden team will move quickly. It’s not like they don’t know what to do.”