I am hearing there is a 4 hour wait to unload ambulances right now.
Ivanka Trump Faces Off With Father to See How Many People They Can Kill With COVID-19
The first daughter, a noted epidemiologist, doesn’t think lockdowns are “grounded in science.”
As you’ve probably heard by now, one of the main reasons COVID-19 was able to gain a foothold in the United States was because Donald Trump ’s approach to the virus was to shamelessly lie about it as it spread throughout the country. After it was here, countless people lost their lives because the president, among other things, let Jared Kushner play a key role in the government’s response to the crisis, which included reportedly cutting doctors and scientists out of the process and effectively declaring mission accomplished in April, before an additional 260,000 people (and counting) would go on to die. (Also unhelpful: the president’s numerous rallies jamming thousands of mostly mask-less people in close proximity, as well as all of his other super-spreader events.) All of which is to say, no one named Kushner or Trump should be allowed to have any say whatsoever when it comes to the U.S.’s COVID-19 measures, a memo that first daughter Ivanka Trump apparently did not get:
Yes, that’s noted epidemiologist Ivanka Trump decrying lockdowns as the country hurtles toward an estimated 450,000 deaths by February 1, a figure that can largely be blamed on her idiot husband and father. While shutdowns have undoubtedly had a catastrophic effect on many businesses, the country wouldn‘t be in the position it’s in now if the Trump administration had taken any of the necessary steps to adequately address the problem—both from a public health and an economic standpoint—or literally done anything to stop the spread of the virus. (As White House chief of staff Mark Meadows told CNN in October, “We’re not going to control the pandemic.”) Incidentally, Ivanka broke federal stay-at-home guidelines in April, because her 8,200-square-foot home had apparently gotten too cramped.
“None of this would even be happening if you had listened to the scientists from the start,“ NYU media research scientist and instructor Justin Hendrix tweeted at the first daughter, “But you didn’t and now…hundreds of thousands are dead and things are happening in local communities that seem chaotic. Don’t blame them for the chain of events you started.” “It will never stop amazing us that in the midst of the worst pandemic in a century, rather than turning to doctors and scientists, the closest advisors to the president were his fashion-brand owning daughter and her slumlord husband,” replied government watchdog Citizens for Responsibility and Ethics in Washington. “This is why we need tighter nepotism laws.” (In reality, Ivanka is a former fashion-brand owner, having shuttered her clothing line in 2018 to focus on her job at the White House doing…well, it’s not actually clear what she does there.)
Not surprisingly, Ivanka, who is known for tweeting context-free bullshit that she thinks helps her image, did not mention that when it comes to the small-business owners she supposedly cares so deeply about, the Trump administration chose not to extend emergency lending programs that benefit those exact people. Or that Treasury Secretary Steve Mnuchin, no doubt with her father’s blessing, is putting hundreds of billions of dollars designated for small- and medium-size businesses into an account where his successor cannot tap them without congressional approval. Or that Trump and Kushner businesses reportedly got millions in PPP loans, while only keeping a handful of employees on payroll. Must have been an honest oversight!
Melania Trump is also so over these attempts not to kill thousands more Americans daily
It’s a family affair, really. Per CNN:
> First lady Melania Trump broke stated mask policy at Children’s National Hospital Tuesday when she removed her mask to read a holiday book to children…. The first lady arrived in the hospital’s main atrium wearing a mask. When she took her seat in front of a tree, she removed the mask. Though she practiced social distancing, the hospital’s policy specifically requires all visitors to wear a mask. “Everyone must wear a mask at all times while in any Children’s National facility to prevent the spread of COVID-19,” the hospital’s policy says.
>
>
>
> Trump was diagnosed with coronavirus at the same time as President Donald Trump in early October. But health experts say it’s still unclear how long antibodies offer protection and recommend still wearing a mask. “Even though the President himself was infected and he has likely antibodies that likely would be protective, we’re not sure how long that protection lasts,” Dr. Anthony Fauci told ABC News on Tuesday.
Melania’s office did not respond to CNN’s request for comment. The Children’s National Hospital treats, in addition to many other things, pediatric cancer, so it’s not like anyone there has a compromised immune system.
Oh look, a Republican has a very racist-sounding thing to say about Reverend Raphael Warnock
In this case it’s U.S. representative-elect for North Carolina’s 11th congressional district Madison Cawthorn, who has previously said that an Asheville proposal for reparations are “racist” because “six-hundred thousand Americans gave their lives to free slaves” and that should be “enough,” a claim that naturally glosses over the fact that more than one third of those soldiers were fighting to maintain slavery. Anyway, Madison over here thinks “this Warnock fella” isn’t a “real” American and that he’s “coming down here and disguising himself as some moderate pastor from the South.” Given that Warnock was born and raised in Georgia, and it’s actually his opponent, Kelly Loeffler, who is from Illinois and didn’t move south until she was an adult, we think this might be a racist dog whistle about Black people not being real Americans (or, apparently, Southerners). But it’s so hard to say given how subtle Cawthorn is being.
Infrastructure Week might happen after all!
Well, there’s bound to be a few of these anomalies.
Alaska Health Worker Had a Serious Allergic Reaction After Pfizer’s Vaccine
The person had no history of allergies. Two similar reactions happened last week in Britain.
A health care worker in Alaska had a serious allergic reaction after getting Pfizer’s coronavirus vaccine on Tuesday and remained hospitalized on Wednesday morning under observation.
The middle-aged worker had no history of allergies, but had an anaphylactic reaction that began 10 minutes after receiving the vaccine at Bartlett Regional Hospital in Juneau, Alaska, a hospital official said. The reaction included flushing and shortness of breath.
Dr. Lindy Jones, the emergency department medical director at the hospital, said the reaction subsided soon after the worker was treated with epinephrine. He said the worker remained enthusiastic that she had received the vaccine and was set to be discharged later on Wednesday.
“She is healthy and she is doing well,” Dr. Jones said.
Some insider’s revelations at the CDC as we are now aware of how the WH and those in charge of dispersing information about Coronavirus took the reigns and closed off communication and facts from CDC. Two political appointees (from Trump) discussed what they witnessed.
Kyle McGowan, a former chief of staff at the Centers for Disease Control and Prevention, and his deputy, Amanda Campbell, were installed in 2018 as two of the youngest political appointees in the history of the world’s premier public health agency, young Republicans returning to their native Georgia to dream jobs.
But what they witnessed during the coronavirus pandemic this year in the C.D.C.’s leadership suite on the 12-floor headquarters here shook them: Washington’s dismissal of science, the White House’s slow suffocation of the agency’s voice, the meddling in its messages and the siphoning of its budget.
In a series of interviews, the pair has decided to go public with their disillusionment: what went wrong, and what they believe needs to be done as the agency girds for what could be a yearslong project of rebuilding its credibility externally while easing ill feelings and self-doubt internally.
“Everyone wants to describe the day that the light switch flipped and the C.D.C. was sidelined. It didn’t happen that way,” Mr. McGowan said. “It was more of like a hand grasping something, and it slowly closes, closes, closes, closes until you realize that, middle of the summer, it has a complete grasp on everything at the C.D.C.”
Last week, the editor in chief of the C.D.C.’s flagship weekly disease outbreak reports — once considered untouchable — told House Democrats investigating political interference in the agency’s work that she was ordered to destroy an email showing Trump appointees attempting to meddle with their publication.
The same day, the outlines of the C.D.C.’s future took more shape when President-elect Joseph R. Biden Jr. announced a slate of health nominees, including Dr. Rochelle Walensky, the chief of infectious diseases at Massachusetts General Hospital, as the agency’s new director, a move generally greeted with enthusiasm by public health experts.
“We are ready to combat this virus with science and facts,” she wrote on Twitter.
Mr. McGowan and Ms. Campbell — who joined the C.D.C. in their early 30s, then left together in August — said that mantra was what was most needed after a brutal year that left the agency’s authority crippled.
A top Trump appointee repeatedly urged top health officials to adopt a “herd immunity” approach to Covid-19 and allow millions of Americans to be infected by the virus, according to internal emails obtained by a House watchdog and shared with POLITICO.
“There is no other way, we need to establish herd, and it only comes about allowing the non-high risk groups expose themselves to the virus. PERIOD," then-science adviser Paul Alexander wrote on July 4 to his boss, Health and Human Services assistant secretary for public affairs Michael Caputo, and six other senior officials.
Seems like Pfizer is ready to go to distribute vaccines, but Operation Warp Speed has not directed the vaccines to go anywhere. Why such a mess? Because it’s the way this administration fumbles all their help to Americans…slowly, and without care. #seePaperTowelToss
Quick replay of where Trump has placed the GOP:
After months of being stalled by Mitch McConnell’s Senate wall, Congress was prepared to pass a new COVID-19 relief bill that only offered $600 per person, far less than Democrats had wanted, but at least something.
Trump then threw a wrench in the works, demanding that they raise the sum to $2,000, perhaps expecting Democrats to automatically oppose it on the basis that the idea came from him.
But it’s what they wanted all along, so they embraced instantly.
Now it’s all on the GOP, who have dragged their feet on this all along. The House has asked for a unanimous consent passage, meaning if the Republicans want to oppose this, one must stand up and do so in person.
Then the bill would go to the Senate where, again, the GOP would have to actively shoot it down, directly defying Trump in the process and setting themselves up before the country as having killed the bill – again.
The Great Negotiator.
How COVID-19 Hollowed Out a Generation of Young Black Men
They were pillars of their communities and families, and they are not replaceable. To understand why COVID-19 killed so many young Black men, you need to know the legend of John Henry.
The Rev. Dr. Kejuane Artez Bates was a big man with big responsibilities. The arrival of the novel coronavirus in Vidalia, Louisiana, was another burden on a body already breaking under the load. Bates was in his 10th year with the Vidalia Police Department, assigned as a resource officer to the upper elementary school. But with classrooms indefinitely closed, he was back on patrol duty and, like most people in those early days of the pandemic, unprotected by a mask. On Friday, March 20, he was coughing and his nose was bleeding. The next day, he couldn’t get out of bed.
Bates was only 36, too young to be at risk for COVID-19, or so the conventional wisdom went. He attributed his malaise to allergies and pushed forward with his second full-time job, as head pastor of Forest Aid Baptist Church, working on his Sunday sermon between naps. Online church was a new concept to his parishioners, and during the next morning’s service, he had to keep reminding them to mute their phones. As he preached about Daniel in the lion’s den — we will be tested, but if we continue to have faith, we will come through — he grimaced from the effort. That night he was burning up with fever. Five days later he was on a ventilator; five days after that, he died.
While COVID-19 has killed 1 out of every 800 African Americans, a toll that overwhelms the imagination, even more stunning is the deadly efficiency with which it has targeted young Black men like Bates. One study using data through July found that Black people ages 35 to 44 were dying at nine times the rate of white people the same age, though the gap slightly narrowed later in the year. And in an analysis for ProPublica this summer using the only reliable data at the time accounting for age, race and gender, from Michigan and Georgia, Harvard researcher Tamara Rushovich found that the disparity was greatest in Black men. It was a phenomenon Enrique Neblett Jr. noticed when he kept seeing online memorials for men his age. “I’ll be 45 this year,” said the University of Michigan professor, who studies racism and health. “I wasn’t seeing 60- and 70-year-old men. We absolutely need to be asking what is going on here?”
To help illuminate this gap in knowledge and gain a deeper understanding of why America has lost so many young Black men to COVID-19, ProPublica spent months gathering their stories, starting with hundreds of news articles, obituaries and medical examiners’ reports, then interviewing the relatives and friends of nearly two dozen men, along with researchers who specialize in Black men’s health. Our efforts led us to a little-known body of research that takes its name from one of the most enduring symbols of Black American resilience.
As the legend goes, John Henry was a steel-driving man who defeated a steam-powered drill and died with a hammer in his hand. The folktale celebrates one man’s victory against seemingly insurmountable odds. But it holds another, harsher truth: His determination and strength are also what killed him. The John Henry of contemporary social theory is a man striving to get ahead in an unequal society. The effort of confronting that machine, day in and day out, compounded over a lifetime, leads to stress so corrosive that it physically changes bodies, causing Black men to age quicker, become sicker and die younger than nearly any other U.S. demographic group. COVID-19 is a new gear in an old machine.
In interviews about the young men who died from the virus, a portrait emerged of a modern John Henry: hard-working, ambitious, optimistic and persistent, trying to lift others along with themselves. They were the very people communities would have turned to first to help recover from the pandemic: entrepreneurs who were also employers; confidants like coaches, pastors and barbers; family men forced into a sandwich generation younger than their white counterparts, because their parents got sick earlier and they had to care for them while raising kids of their own.
They were ordinary men. Time and again, it was their fight that was remarkable.
Kejuane Bates and his daughter, Madison.
Bates, the only child of a single mother who supported him as a teacher’s aide, made it to Alcorn State University on football and choir scholarships. When his mother got sick with breast cancer, he had to drop out; after she died, he was almost destitute. Over the years, he built himself into multiple men at once, each a pillar to many others: the pastor whose flock depended on his counsel; the mentor known to school kids as Uncle Officer Bates; the assistant football coach and band director; the adoring father to 5-year-old Madison — his “heartbeat,” he called her. Recently he and his wife, Chelsea, a second grade teacher, had launched One Love Travel, organizing excursion packages and cruises as part of their long-term plan to build generational wealth.
He carried the stress of his efforts in his blood vessels, in his kidneys, in the extra pounds that accumulated with each passing year; he had diabetes and hypertension and at 6-foot-6, he was more than 100 pounds overweight. His official cause of death, on April 1, was COVID-19-related pneumonia and acute respiratory distress syndrome.
But Chelsea knows that the virus, no matter how powerful, didn’t kill her husband on its own. It was the years of working nonstop, taking care of other people more than himself, that wore his body down. And when the virus attacked, he couldn’t fight back.
In the summer of 1978, the social epidemiologist Sherman James, then a 34-year-old researcher at the University of North Carolina at Chapel Hill, met the man who would shape his life’s work. At 70, John Martin was a retired farmer who suffered from debilitating osteoarthritis and hypertension. He had peptic ulcers so severe that doctors had to remove 40% of his stomach. Recounting his story in his backyard rocking chair, his cane resting on his lap, the old man had no doubt why his health was so bad: “I worked too hard.”
Born in 1907, Martin grew up in a family of sharecroppers who were only paid half of what their labor in the tobacco fields earned. Throughout the South at the time, most Black farmers lived at the economic mercy of landowners who were employers, landlords and vendors all at once. Martin watched as the system ruthlessly exploited his father; after one particularly harsh winter spent hungry, Martin vowed he would be different. Borrowing $3,725 in 1941, he purchased 75 acres. He had 40 years to settle the mortgage but accomplished the near-impossible: He paid it off in five. “That’s the reason my legs [are] all out of whack today,” he told James.
James listened, spellbound, until Martin’s wife called out, “John Henry, it’s time for lunch.” At that moment, something clicked. Holy cow, James remembers thinking. “It was just like the ancestors were speaking to me.” The power of Martin’s story wasn’t simply that it echoed the legend of John Henry; it also echoed the life experiences of most of the working-class African American men James knew.
Five years out of graduate school, James was among a small group of researchers focusing on one of the most enduring public health problems in the United States: why health outcomes for Black men are so poor. Black men live shorter lives than all other Americans — 71.5 years versus 76.1 years for white men — and have for generations. Black men’s life expectancy didn’t reach 65, the eligibility age for Medicare, until 1995, 30 years after the federal health program for the elderly became law; white men were living into their mid-60s by 1950. The shorter lifespans reflect a broader disparity: Black people have much higher rates of hypertension, obesity, diabetes and strokes than white people do, and they develop those chronic conditions up to 10 years earlier. The gap persisted this year when the Brookings Institution examined COVID-19 deaths by race; in each age category, Black people were dying at roughly the same rate as white people more than a decade older.
For generations, public health experts mostly ignored the disparities. When they did pay attention, they invariably blamed the victims — their “unhealthy” behaviors and diets, their genes, the under-resourced neighborhoods they “chose” to live in and the low-paying jobs they “chose” to work. Their chronic illnesses were seen as failures of personal responsibility. Their shorter life expectancy was written off to addiction and the myth of “black-on-black” violence. Many of those arguments were legacies of the slave and Jim Crow eras, when the white medical and science establishment promoted the idea of innate Black inferiority and criminality to rationalize systems built on servitude and segregation.
Pondering the lessons of John Henry Martin, James began to see what many of his colleagues had been missing. It wasn’t just living in poverty that wore down Black men’s bodies, he hypothesized, but the struggle to break out of poverty. It wasn’t just inequality that made them sick, but the effort to be equal in a system that was fundamentally unjust. “It’s this striving to make something of themselves … to live their lives with dignity and purpose and to be successful against extraordinary circumstances,” James said. “They’re trying to make a way out of no way. It’s the Black American story.”
America has changed profoundly since Martin’s day. Yet the machinery of racial inequality continues to be omnipresent. It’s in the hospitals where Black newborns double their chances of surviving if they’re cared for by Black doctors rather than white ones. In the redlined neighborhoods where poverty and pollution are concentrated — but not affordable housing or grocery stores or reliable internet. It’s in the crumbling, exploitative economies that force parents to risk their lives working long hours for low pay without sick leave. In mass incarceration and voter suppression. In the innumerable hurdles, one piled upon another, that make Black Americans’ climb up the socioeconomic ladder more daunting than ever, their successes more fragile and their setbacks more consequential.
“Everyone thinks about racism as something that is personally mediated, like someone insulting me,” said Linda Sprague Martinez, a professor at Boston University’s School of Social Work who conducts community health research with adolescents and young adults. “But the way in which it’s really pervasive is how it disrupts life chances and opportunity. … These are systems that are designed for you to fail, essentially, and for you to be erased and to be maintained in a certain position in our society.”
Challenging such a relentless machine, through “high-effort coping,” James concluded, requires three categories of personal traits that are major themes of the John Henry legend: tenacity, mental and physical vigor and a commitment to hard work. To measure them, he developed the John Henryism scale, with scores determined by how strongly people identify with 12 statements, including: “Once I make up my mind to do something, I stay with it until the job is completely done,” and, “It’s not always easy, but I usually find a way to do what really needs to be done.”
To score high in John Henryism, you don’t have to be Black or male or economically disadvantaged. But over the years, James and other researchers have found that Black people, especially those who are poor and working-class, do score high and tend to suffer greater cardiovascular risks, perhaps because the innumerable hurdles in their paths require greater effort to overcome. “The stress,” James said, “is going to be far more overwhelming than it has a human right to be.”
Stress is a physiological reaction, hard-wired in the body, that helps protect it against external threats. At the first sign of danger, the brain sounds an alarm, setting off a torrent of neurological and hormonal signals that whoosh into the blood, stimulating the body to fight or give flight. The heart beats faster and breathing quickens; blood vessels dilate, so more oxygen reaches the brain and muscles. The immune system’s inflammatory response is activated to promote quick healing. When the threat passes, hormone levels return to normal, blood glucose ebbs and heart rate and blood pressure go back to baseline. At least, that’s how the human body is designed to work.
But overexposure to cortisol and other stress hormones can cause the gears to malfunction. “Your body’s over-producing, always working hard to bring itself back down to the normal level,” said Roland J. Thorpe Jr., a professor at the Johns Hopkins Bloomberg School of Public Health and founding director of the Program for Research on Men’s Health at the Hopkins Center for Health Disparities Solutions. The constant strain “resets the normal,” he said. As blood pressure remains high and inflammation becomes chronic, the inner linings of blood vessels start to thicken and stiffen, which forces the heart to work harder, which dysregulates other organs until they, too, begin to fail. “Your body starts to wear down,” Thorpe said — a phenomenon known as weathering.
The cumulative effects of stress begin in the womb, when cortisol released into a pregnant woman’s bloodstream crosses the placenta; it is one of the reasons a disproportionate number of Black babies are born too early and too small. Then, exposure to adverse childhood experiences — anything from abuse and neglect to poverty and hunger — continues the toxic stream; too much exposure to cortisol at a critical stage in development can rewire the neurological system’s fight-or-flight response, essentially causing the brain’s stress switch to break. The more stress a youngster endures, the more likely he or she is to have academic, behavioral and health problems from depression to obesity.
Weathering isn’t specific to race, but it is believed to take a particular toll on Black people because of the unique, unrelenting stress caused by racism that wears away the body and the spirit, “just like you have siding on the house, and the rain or the sun beats on it, and eventually it starts to fade,” said Dr. Jerome Adams, the U.S. surgeon general under the Trump administration. Shawnita Sealy-Jefferson, a social epidemiologist at Ohio State University, says the human body isn’t designed to withstand such biological and emotional assaults: “It’s the same thing as if you revved the engine of your car all day, every day. Sooner or later, the car is going to break down.”
The effects of stress can be seen at the cellular level. Researchers have found that in Black people, telomeres — repeated sequences of DNA that protect the ends of chromosomes by forming a cap, much like the plastic tip on a shoelace — become shortened at a faster rate, a sign of premature aging. In a 2018 study examining changes in seven biomarkers in cardiac patients over a 30-year period, researchers found that Black patients weathered at an average of about six years faster than whites. And it was the extraordinarily high rates of hypertension in the Black community that prompted scientists to look at the impact of stress in the first place. By age 55, about 76% of Black men and women develop high blood pressure, versus 54% of white men and 40% of white women, which increases the risk of heart attacks and strokes.
Sustained stress has strong links to obesity, which Black children and adults have at much higher rates than whites. Some of this is physiological: The interplay between cortisol and glucose is complex and insidious, triggering metabolic changes that can lead to diabetes and other chronic diseases. Some of it is psychological and behavioral: Stress is strongly associated with depression and other mental health disorders. “The way that people deal with stress is by strategies that make us feel better,” such as comfort eating, said Thomas LaVeist, dean of Tulane University School of Public Health and Tropical Medicine. Stress and anxiety cause sleeplessness, which itself is correlated with weight gain. The result is often a cascade of health problems — hypertension, cardiovascular disease, metabolic syndrome — that strike early and feed off of each other.
Because Black Americans experience many forms of stress, often at once, researchers have more questions than answers about the specific role John Henryism plays in these outcomes. The study of Black men’s health remains an under-examined frontier, with little in the way of funding or will because “Black men are not viewed as sympathetic,” said LaVeist, and because so few go into the health research professions. He and Thorpe, the Johns Hopkins professor, co-founded the Black Men’s Health Project, the first large-scale national study focused solely on Black men’s needs, with a goal sample size of 5,000. They hope to learn how stressors like segregation and adverse early life experiences impact health outcomes.
If this segregated body of emerging knowledge were to grow and infiltrate the mainstream medical and research communities, James can only imagine how beneficial that would be. Health professionals could build deeper relationships with their patients by better understanding the sources of stress that wreak havoc on their cardiovascular systems. They could test for high blood pressure, diabetes and cholesterol levels more frequently and at younger ages. “Until we can have a society that is more just racially,” James said, “we do need to find these intermediate steps.”
As ProPublica examined the lives lost to COVID-19, themes emerged in the pressure points faced by many young Black men. The wearing down typically begins when they are boys and must become little John Henrys to navigate white spaces or push through the adverse experiences endemic to Black communities. It continues when they grow into men, as most need to navigate the public’s projections of danger with unwavering vigilance. The more they succeed, the more responsibility they feel to lift their families and communities with them, and with that, comes more stress.
As James listened to the stories ProPublica was gathering, he instantly recognized the cycle of striving and succumbing that he has been writing about for 40 years. “They could have done so much more had the struggle not been so intense,” James said. “They were cut down too soon.”
Thomas Fields Jr. was barely a year old when his father first went to prison. The loss altered the trajectory of his life in ways that many children wouldn’t have been able to overcome. His mother, just 17 when he was born, moved with him from the suburbs of Washington, D.C., to Detroit, where her own mother had recently relocated. The city was in freefall: manufacturing jobs were disappearing; crime was surging; middle-class and white flight was stripping away the city’s tax base, eroding vital services and causing schools to fail. Just waiting at the wrong bus stop could get you robbed or shot.
“When you’re a young male living in Detroit, if you live past 18, it’s like you’re 50 years old,” Fields, then 31, said on a Facebook Live chat last year. “I swear that’s how it feels.”
Mitigating childhood adversity requires deep wells of resilience; researchers say one of the best ways to build those reserves is having a nurturing caregiver. In this, young Thomas was exceptionally lucky. His mother worked two jobs and still managed to watch him like a hawk; she told him constantly that she loved him. His grandmothers looked after him after school and during summer breaks. His father, Thomas Sr., did his best to be involved from behind bars, urging him to not make the same mistakes. “I wanted this Thomas Fields to break the mold,” he said.
Thomas Fields Jr. (Courtesy of Fields’ family)
To do that, Thomas became a little John Henry. He got decent grades, stayed out of trouble and taught himself to cook — healthy food, not the junk so many of his peers ate. After high school, he attended Grambling State University in Louisiana for a couple of years, then joined the U.S. Navy, where he went from being a talented amateur chef to a trained professional. He also became a father. When there were setbacks, he was already planning his next move. It’s a strategy that Black adolescents absorb like the air they breathe and the water they drink, Sprague Martinez said. “The mentality is: ‘Even if this system is not designed to work for me … I’m going to win this game. I haven’t gotten the prize yet? I must not be working hard enough.’”
High-effort coping can confer mental health benefits even for children raised in the direst of circumstances. Dosha DJay Joi endured the kind of trauma that dooms many children — beatings, neglect, sexual abuse. Born in Chicago, he spent much of his adolescence in group homes in the Wisconsin system. For years he was afraid to talk about the abuse and scared to tell his birth mother he was queer. He learned to channel himself into education and advocacy, helping other LGBTQ and foster kids; he especially wanted to make sure children remained connected with their siblings. He was inspired to study social work because of what he’d been through, said his mother, Kecha Kitchens. “Then a family member got sick, and he didn’t like how the nurses were treating the other patients in the nursing home, so he wanted to become a nurse.”
Dosha Joi. (Courtesy of Kecha Kitchens)
By the age of 28, Joi had a bachelor’s degree in human services, he had trained as a substance abuse counselor and he was working toward his nursing degree. He served as a court-appointed special advocate for kids aging out of foster care and lobbied lawmakers in the Wisconsin capitol and Washington D.C., forming a special bond with Rep. Gwen Moore, who represents Milwaukee in Congress. But the years of hardship took an enormous physical toll; Joi suffered from hypertension, heart and lung problems and at his heaviest, he weighed more than 500 pounds. When COVID-19 arrived in the Midwest, he was particularly vulnerable. He died on May 14.
For young John Henrys, the psychological benefits of high-effort coping seem to be complicated by what’s happening inside the body. “Typically when you study resilience in any group, and [subjects are] doing well by our typical metrics” — going to college, getting a good job, not taking drugs — “we say, ‘Woo-hoo,’” University of Georgia researcher Gene Brody said. “Logically, we thought this would transfer to have health benefits.” But for Black young adults trying to climb the economic ladder, they found just the opposite. “When you look under the skin, doing blood draws and using other kinds of measures, they look like their health is starting to suffer.”
In more than 25 years spent tracking the health of Black families in rural Georgia, Brody and his colleagues found that adolescents identified by their teachers as being success-oriented already had higher “allostatic loads” — science jargon for wear-and-tear on the body — at age 19 than their peers. By age 25, those from more disadvantaged backgrounds who scored high on the John Henryism scale were more likely to have metabolic syndrome, a cluster of conditions that are precursors to diabetes and heart disease, than people from less disadvantaged backgrounds. Brody and his colleagues have dubbed this phenomenon “skin-deep resilience.” The same effects are not found for young white strivers.
In his late 20s, Fields was diagnosed with such a severe case of diabetes that his military career came to a screeching halt. When he returned to Detroit last year, he was a little brawnier, with more tattoos. “Diabetes was something that he was going to beat, because he wasn’t going to lose to anything,” said the Rev. Torion Bridges, one of his best friends for 20 years. He became a personal chef and motivational speaker, started a podcast and wrote a cookbook. He helped out his mom, who had multiple sclerosis. And he took a job as a “school culture facilitator,” working with kids who had discipline problems, at Paul Robeson Malcolm X Academy, the pioneering Afrocentric public school he had attended. He was especially good with troubled boys who didn’t have a father at home, said principal Jeffrey Robinson, his onetime homeroom teacher, later his boss. “He could identify with the feeling of the loss.”
In March, Fields and his mother caught the coronavirus at the same time.
She recovered. He did not.
To navigate life as a Black man is to be constantly vigilant. The ubiquity of racism means that everyday interactions, while driving or shopping or birdwatching, can have potentially dangerous outcomes. So John Henrys live in a heightened state of awareness, continually adjusting. It might mean placing family photos near the front door to quickly prove your son belongs should police ever respond. It often means being able to “strategically assimilate” — to assume a public identity aimed at neutralizing stereotypes of blackness and defusing irrational white fears. This, W.E.B. DuBois explained more than a century ago, is “double-consciousness, this sense of always looking at one’s self through the eyes of others, of measuring one’s soul by the tape of a world that looks on in amused contempt and pity.”
New York Times columnist Brent Staples would whistle Vivaldi in graduate school to signal that he was too cultured to be threatening. Darrell Hudson, who researches health disparities at Washington University in St. Louis, scans the closet each day before teaching class to select what he calls his “Non- Threatening Black Guy Uniform.”
“What’s not appreciated fully, I think, is how much energy it takes,” said Derek M. Griffith, professor and director of the Center for Research on Men’s Health at Vanderbilt University. “All of these different things that you have to do to modulate your body and so forth, all that additional attention that you have to pay to that, is a burden that most people don’t have to bear. It is a cause of weathering that we don’t fully appreciate.”
A 2014 study found that vigilance was positively associated with the prevalence of hypertension for Blacks but not whites. The more vigilant Black people were, the more the disparity grew. And researchers have found that Black people who are on guard against anticipated discrimination have higher blood pressures while they sleep. “When you experience racism or discrimination and it could cost your life, it’s good to be vigilant; but a prolonged and heightened state of vigilance is not good,” the University of Michigan’s Neblett said. “It can kill you in the end.”
Leslie Lamar Parker, at a maternity photo shoot before the birth of his son Chance. (Courtesy of Whitney Parker)
Leslie Lamar Parker grew up in the Minneapolis suburbs, in a state that was 84% white. Like many John Henrys in this story, he was large — tall and wide — in a way that made him stand out to cruel classmates and clueless teachers. Bigness can be perilous for Black boys, who are often seen as older, stronger and less innocent than their white counterparts, stereotypes that underlie higher rates of school discipline and police violence. Parker learned to play the class clown and questioned authority. “School couldn’t hold his attention, not because he wasn’t smart. He wouldn’t go,” his mother, Tyuon Brazell, said. Because he wasn’t on track to graduate, she did what other parents might not and suggested he drop out his junior year. That’s when he started to thrive, earning his GED, graduating from college and becoming an IT specialist in his old school district, where he mentored students of color, ordering them lunch from DoorDash and supervising the tech club. “That was really important to him,” said his wife, Whitney, “making sure they didn’t fail any other brown kids like they failed him.”
One key to his coping was overcorrecting for how he might be perceived. Strangers would approach him to say how lovely it was to see him with his son and daughter, a microaggression masquerading as a compliment. He was so sensitive to stereotypes about absent Black fathers, his wife said, he was “a present parent on steroids.” To walk through the world as a Black man is to be simultaneously hypervisible and invisible, under surveillance yet never really seen. So he turned his wardrobe into a “conversation starter,” an expression of his irreverent personality but also armor against snap judgments about his imposingness. He carried a Spongebob SquarePants backpack to work and often wore a pro-wrestling or superhero T-shirt during off hours.
Parker was constantly scanning the horizon for threats against his family and his kids at school, wondering whether there was something more that he could do for them. He projected a cool demeanor, his argumentative wit camouflaging worries that his mother knew kept his head in overdrive. “I kept telling him: ‘Son, you need to rest. You don’t have to do everything in a day.’” He was diagnosed with high blood pressure at just 27 and worried it, and the extra pounds, would keep him from seeing his two children grow up. He died in May from COVID-19 at the age of 31.
The effort it takes for Black people to navigate mostly white spaces — to get an education, earn a living, take out a loan, raise a child — can be caustic. Their credentials are questioned; expertise doubted. On college campuses, Black students are often asked if they’re on a sports scholarship or if they’re really students. Research shows that a person doesn’t need to be the target of a racist incident for his body to be affected. Watching videos of police killing Black people or even just anticipating a racist experience can trigger the fight-or-flight response. Incidents build up in memories and transform into chronic stressors; ruminating on them can activate the body’s biological stress reaction. This happens over and over again, often many times a day, until the cortisol pump essentially breaks.
Joshua Bush. (Courtesy of LaKita Bush)
Joshua Bush, who died in April of COVID-19, slammed up against racial stereotypes in his work as a nurse in South Carolina. There were funny looks from people who didn’t expect to see a Black man when he arrived at job interviews and white patients who refused to let him touch them. He told them, “That is your choice, but you’re missing out on great help,” his mother, Linda, recalled. He and his wife, LaKita, saw the health care industry as their route to upward mobility. She worked in hospital administration; at 30, he was studying to become a registered nurse, working as an LPN.
Bush also suffered from a rare enzyme abnormality that caused severe muscle cramps from overexertion, and because of it, trips to the emergency room weren’t uncommon. He’d come to accept that the first image doctors and nurses saw — someone Black and overweight — influenced their bedside manner. They treated him like he had no medical knowledge and lectured him about diabetes, though it had nothing to do with why he was seeking care. His experience informed the way he cared for his own patients, part of his “fight against the system,” his wife said. At the same time, she could see her husband’s stress “all over his body.”
Lifting as we climb, onward and upward we go. Words that started as a call-to-action at the rise of the Jim Crow South have become an enduring part of the African American experience — and can serve as a unique form of stress. The proverb was born of Black suffragist Mary Eliza Church Terrell’s belief that it was incumbent upon the growing Black middle and upper class to use their position to fight racial discrimination and help others rise through education, work and community activism. It is why Thomas Fields was told as a boy that he was “duty-bound” to give back to the community once he got an education. Why Dosha Joi advocated for young people in the system “because someone helped bring out the sunshine in me.”
“You’re socialized to say it’s not just about you. It’s really about what you’re going to do for your broader community and for your family,” Washington University’s Hudson explained. “People take it very seriously, trying to light a path for those behind them — even when they’re not necessarily in the most stable situation themselves. … But they’re lifting as they climb. That’s taxing. That’s a visceral stress.”
In the Brookhaven, Mississippi, of Eugene Thompson’s youth, Black business owners understood that Brookway Boulevard — at least the stretch that ran through downtown — was for white businesses. The election of Barack Obama was a turning point; Thompson figured if a Black man could become president of the United States, surely he could rent a modest space on “the Boulevard.” Publicly, his goal was to grow his client base by cutting white people’s hair, too. His family knew his aspirations were grander. “He wanted to do something in Brookhaven to help Black people to get off their knees,” his mother, Odell Edwards, said. “We are on our knees.”
It’s not easy earning a living in Mississippi, where the single most common job is working as a cashier and the $7.25 minimum wage hasn’t budged in a decade. Cutting hair came naturally for Thompson, who started on himself at 12. He attended a local beauty academy before he could afford to go to barber school and over the years took the same methodical approach to growing his business — buying secondhand equipment, doing the construction himself, all without bank loans, mentoring or government support.
Eugene Thompson. (Courtesy of Odell Edwards)
But Thompson’s real ambition was to start his own school. “He always tried to encourage the boys in the community, or people who had been in prison and couldn’t find a job — ’I can teach you how to cut hair and you can have your own business,’” his younger sister, Dedra Edwards, said. After three years spent earning his teaching credential, Thompson opened his TaperNation Barber Academy for students last fall. Then he realized graduates needed places to work, so he launched his next project: renovating a second shop nearby where other barbers and hair stylists could rent chairs.
“It was running him ragged,” Odell said.
At 46, Thompson was severely overweight and suffered from lifelong respiratory problems as well as anxiety and sleeplessness. High blood pressure and diabetes ran in his family, but Thompson’s true health status was unclear — like more than 15% of Black people in Mississippi, he wasn’t insured and avoided going to the doctor except in an emergency. When he started feeling symptoms of COVID-19 in late March, he shrugged them off at first; he’d been having heart palpitations and panic attacks, which his family attributed to stress from work.
After he died in early April, leaving behind six children, TaperNation had to shut down. “You have to have a barber’s instructor license to keep it going, and no one else in the family has one,” his sister said. “We had to sell almost everything.”
Recent disasters — Hurricane Katrina, the Great Recession — have shown that Black communities aren’t just more vulnerable than white populations to economic and social dislocations; they recover more slowly. The impacts of the pandemic are likely to be magnified because so many deaths have occurred among Black people under age 60, the peak earning years when people raise families, start businesses, amass social capital and create lasting legacies. In addition to the lives it took, COVID-19 has robbed wealth that John Henrys were only beginning to accrue and toppled what they had begun to build for themselves and those around them.
In many cases, they were the structural beams, holding everything up. “These are people who help pay bills for people who aren’t their biological family members,” said Sealy-Jefferson, the Ohio State social epidemiologist. “They bring food when somebody dies. They watch kids when a single mother has to work.” Some of the biggest losses are intangible, she said: “social support, emotional support, resource sharing, encouragement, storytelling, role modeling— all of these things that are vital for African Americans in particular, given our history in this country.”
Fields couldn’t comfort students reeling from a crisis that has killed more than 1,600 of their loved ones and neighbors. “It’s a tremendous loss,” said Robinson, his principal. Bates’ wife, Chelsea, was too bereaved to go back to work when school resumed, which meant living off of her husband’s death benefits and savings; she focused on trying to help Madison process a grief she’s too young to understand. “Sometimes she lays on the floor and kicks and screams that she wants her daddy, that she misses daddy and why did he have to leave?” she said. “I tell her, I’m sorry, I wish that mama could do something to bring him back. I really do.”
Weekday mornings have been quiet without Kendall Pierre Sr. puttering around the house before sunrise so he could open his barbershop by 5 a.m. That’s when workers from nearby chemical plants would stop in for a cut or shave after their graveyard shifts. Sundays are different without his sermons at Mt. Zion Baptist Church, in the little town of Ama, Louisiana, followed by a family breakfast his son always looked forward to. “My grandmother would come. Some of my aunties and cousins. He would put Aunt Jemima batter in the waffle iron and say: ‘See? This is better than Waffle House!’”
Since his dad died in May of COVID-19, Kendall Pierre Jr., a 20-year-old student at Louisiana State University, has felt an overwhelming absence and, at the same time, his father’s equally consuming presence. “I can still hear him,” he said.
Clockwise from left, Kendall Pierre Sr., sons Kaden and Kendall Jr., wife Sabrina and daughter Tayler. (Courtesy of Sabrina Pierre)
Don’t drive with your hoodie on.
Work twice as hard.
Real men don’t wear slippers in public; put on some shoes.
The only child of a single mother, 45-year-old Pierre Sr. took his role as father figure seriously. To nieces and nephews, he was Uncle Dad. To his sons’ basketball teams, he was Coach Kendall with the pep talks.
If a task has begun, never leave it until it’s done.
Be the labor great or small, do it well or not at all.
When players couldn’t afford uniforms or travel for tournaments, he would pay. “Their parents would send them with all they could, which was sometimes only $5,” Pierre Jr. said. They could count on him for food, deodorant, even a haircut. “He would bring his clippers to make sure all the players looked nice.”
When the killing of George Floyd roiled the country, Pierre Jr. had no doubt about how his father would have reacted. He would have talked to officials at the sheriff’s office, school board administrators, government leaders. He would have organized community meetings at the church.
We’re living in troubled times.
His son thought about that when his friend texted him about organizing a Black Lives Matter protest. “Since my dad passed, I’ve had this newfound courage, and this urge to act on things … to just do things outside of my comfort zone,” he said.
On a Saturday morning in June, 400 people joined in the 2.6-mile march from Westbank Bridge Park to St. Charles Parish Courthouse. A local reporter covered it and interviewed Pierre Jr. for a story. “If we don’t speak about systemic racism and police brutality, no change will ever happen,” he said. “I feel like it’s something that I have to do and be a part of something bigger than just me.”
He knows his father would have been proud. His mother was. But she worries, too. Her husband didn’t make enough time for doctor’s appointments to monitor his Type 2 diabetes, nor did he get much sleep. “I would tell him, ‘Kendall, you need to rest,’” recalled Sabrina, his wife of 24 years and a registered nurse. “He would say he could rest when he’s dead and gone.”
She knows how much goes into taking care of yourself as a Black man and thinks about that every time her sons walk out the door; her daughter, too. “Lord, I pray for them. … I tell them: ‘Put the seat belt on, drive the speed limit. Make sure you don’t get any tickets.’ I don’t want them to get stopped by a cop.” Her husband’s stature in the community conferred a kind of protection. “Because of my husband and who he was, people would be looking out for my sons. We don’t have that anymore.”
With vaccines entering into the picture, and at least one-third of people are hesitant to take it, Dr. Fauci has raised the numbers of total vaccinated for better herd immunity. - now between 75 - 80%
Since the start of the pandemic, the figure that many epidemiologists have offered has been 60 to 70 percent. That range is still cited by the World Health Organization and is often repeated during discussions of the future course of the disease.
Although it is impossible to know with certainty what the limit will be until we reach it and transmission stops, having a good estimate is important: It gives Americans a sense of when we can hope to breathe freely again.
Recently, a figure to whom millions of Americans look for guidance — Dr. Anthony S. Fauci, an adviser to both the Trump administration and the incoming Biden administration — has begun incrementally raising his herd-immunity estimate.
n the pandemic’s early days, Dr. Fauci tended to cite the same 60 to 70 percent estimate that most experts did. About a month ago, he began saying “70, 75 percent” in television interviews. And last week, in an interview with CNBC News, he said “75, 80, 85 percent” and “75 to 80-plus percent.”
…>
Asked about Dr. Fauci’s conclusions, prominent epidemiologists said that he may be proven right. The early range of 60 to 70 percent was almost undoubtedly too low, they said, and the virus is becoming more transmissible, so it will take greater herd immunity to stop it.
Dr. Fauci said that weeks ago, he had hesitated to publicly raise his estimate because many Americans seemed unsure about vaccines, which they would need to accept almost universally for the country to achieve herd immunity.
Remember the “Russian vaccine” and how they had it under control?
Turns out Russia’s been lying about its COVID numbers, of course.
The state statistics agency reported over 200,000 more deaths up to November than in 2019, which a senior official attributed largely to the coronavirus, even as the official count remained below 60,000.
Louisiana GOP Congressman-Elect Luke Letlow, age 42, Dies From COVID-19
Dawn Wells, ‘Gilligan’s Island’s’ Mary Ann, Dies of COVID at 82
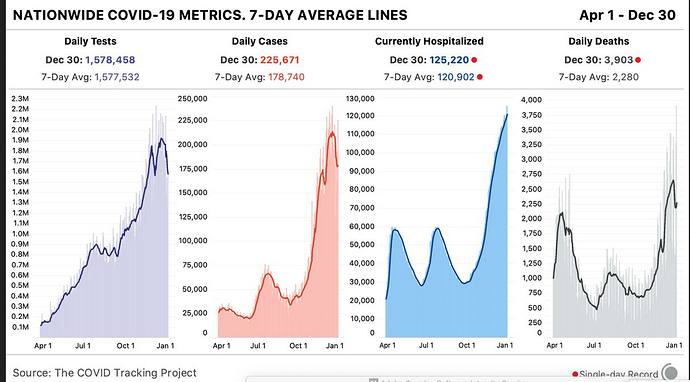
Daily numbers are horrendous…and death total nears 4,000. 
https://pbs.twimg.com/media/EqhsMLKUUAIeqae?format=jpg&name=large

Rogue Pharmacist Arrested After 57 People Get Compromised Vaccine
Another stumbling block into getting the vaccine out…frontline workers who refuse to get vaccinated.
They are frontline workers with top-priority access to the COVID-19 vaccine, but they are refusing to take it.
At St. Elizabeth Community Hospital in Tehama County, fewer than half of the 700 hospital workers eligible for the vaccine were willing to take the shot when it was first offered. At Providence Holy Cross Medical Center in Mission Hills, one in five frontline nurses and doctors have declined the shot. Roughly 20% to 40% of L.A. County’s frontline workers who were offered the vaccine did the same, according to county public health officials.
So many frontline workers in Riverside County have refused the vaccine — an estimated 50% — that hospital and public officials met to strategize how best to distribute the unused doses, Public Health Director Kim Saruwatari said.
The vaccine doubts swirling among healthcare workers across the country come as a surprise to researchers, who assumed hospital staff would be among those most in tune with the scientific data backing the vaccines.
The scientific evidence is clear regarding the safety and efficacy of the vaccines after trials involving tens of thousands of participants, including elderly people and those with chronic health conditions. The shots are recommended for everyone except those who have had a severe allergic reaction to any of the ingredients.
Still, skepticism remains.
…
“I’m choosing the risk — the risk of having COVID, or the risk of the unknown of the vaccine,” Lu said. “I think I’m choosing the risk of COVID. I can control that and prevent it a little by wearing masks, although not 100% for sure.”
Some of her co-workers have also declined to take the vaccine because they’ve gone months without contracting the virus and believe they have a good chance of surviving it, she said. “I feel people think, ‘I can still make it until this ends without getting the vaccine,’” she said.
It’s NYC all over again.
California funeral homes run out of space as COVID-19 rages
From the NYT Coronavirus newsletter NYT Coronavirus debrief
- Prime Minister Boris Johnson closed schools and declared a strict national lockdown in England in an attempt to contain a more contagious variant.
- A pharmacist at a Wisconsin hospital, an “admitted conspiracy theorist,” destroyed 500 doses of coronavirus vaccine because he thought they weren’t safe, police said.
- India approved a locally made vaccine, as well as one made by Oxford-AstraZeneca, for emergency use.
- In the United States, over 20.7 million people have tested positive and at least 352,397 have died. Get the latest updates here, as well as maps and news on vaccines in development.
The vaccine blame game
In the week since our last newsletter, U.S. distribution of coronavirus vaccines has descended into turmoil. Now, millions of vaccines could expire before they reach people in need.
The Trump administration predicted 20 million people would receive at least one dose of a Covid-19 vaccine by the end of 2020. The final figure was about four million. And only 365,294 people in nursing homes and long-term-care centers have been vaccinated, despite more than 2.5 million doses distributed for those facilities, the Centers for Disease Control and Prevention reported.
Critics say the U.S. government has mismanaged the rollout from top to bottom. Federal, state, and local officials blamed each other for botched logistics and funding shortfalls.
State officials — struggling to handle outbreaks, mass testing campaigns, overflowing intensive care units and uncertain contact tracing — say they need more help from the federal government. And local governments are chafing at state restrictions.
In New York City, only 110,000 people have received a vaccine dose — about a quarter of the total number received by the city. Mayor Bill de Blasio called on the state government — which has limited vaccinations to health care workers and those living and working at nursing homes — to allow older people and essential workers to receive the vaccine.
Gov. Andrew Cuomo asserted that the problem was a local issue, and urging Mr. de Blasio and other local leaders to take “personal responsibility” for their performance. Mr. Cuomo also threatened to fine hospitals if they did not step up the vaccination rate.
The $900 billion federal pandemic relief package will provide an additional $9 billion toward vaccination costs. But funds will arrive long after local health departments have started vaccinating residents. Slowdowns touch almost every part of the country.
- In Puerto Rico, a shipment of vaccines did not arrive until the workers who would have administered them had left for the Christmas holiday.
- In Houston, the city health department’s phone system crashed on the first day of a free vaccination clinic, after receiving more than 250,000 calls.
- In Tennessee, older people lined up on a sidewalk, leaning on walkers and wrapping themselves in blankets while they waited for a county health department to open its free clinic. The clinic exhausted its supply of vaccine before 10 a.m.
- In Florida, vaccine rollout sites continue to be overwhelmed in some places, with people waiting for hours. Gov. Ron DeSantis said hospitals may have future supplies of coronavirus vaccine reduced if they do not administer doses quickly enough.
The U.S. is not alone: The Netherlands and France are just two of several countries that have been slow to roll out vaccinations. But the level of disorder in the U.S., as with the virus’s toll, seems unique.
You can follow the U.S. rollout with our vaccine tracker.
Why?
==================================
The thing to remember about this case is that she had not had the second shot, and they’ve been uncertain if the vaccine will prevent it entirely or simply mitigate the worst symptoms. So it’s not necessarily a bad sign for the vaccine, but it may be for convincing people that it’s effective.
Agree with you here…I was so alarmed at first, but obviously the 2nd shot would be the reinforcement for protection we hope.
And yes…people could be just looking for the excuse not to take it.
It’s a red (possibly purple) state Texas. They have their own version of what Covid is, and what the vaccine may do according to their information channels, and spokespeople.